Although chronic total occlusion (CTO) is a common finding, there is little consensus as to when such lesions should be treated routinely with angioplasty.
Benefits of successful rechanneling include relief of symptoms, resolution of ischemia, improvement in ventricular function, and avoidance of myocardial revascularization surgery.
Unsuccessful rechanneling is common and may be associated with several adverse events, such as excess contrast and radiation exposure, coronary perforation, and even cardiac tamponade and death.
Traditional rechanneling techniques offered success rates ranging from 60% to 75%, much lower than rates for conventional angioplasty. Nowadays, with contemporary techniques and more-experienced trained operators, success rates may range from 80% to 90%.
Also read: “Successful CTO Reduces Local and Remote Residual Ischemia”.
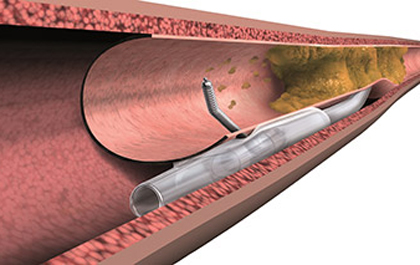
The major barrier for success is the inability to traverse the occluded segment with a guidewire due to fibrotic, calcified tissue, and no well-defined distal lumen.
Different techniques have tried to bypass the problem, for example, the intentional use of extraluminal space to gain access to the true lumen after obstruction. This technique is known as antegrade dissection and reentry, and it involves a potential risk of loss of lateral vessels that may be in the way.
Retrograde access is even more challenging, but remains a fundamental tool for expert operators. In this case, the lesion is penetrated from the distal part, which is accessed through collateral channels.
There may even be a need for controlled extraluminal antegrade and retrograde access, in which a balloon inflated in the antegrade extraluminal space generates room enough for the retrograde guidewire to reach the true proximal lumen.
Also read: “CTO in Patients with Acute Myocardial Infarction Increases Mortality”.
Many devices used in CTOs are uniquely designed for this procedure and extremely unfamiliar for conventional operators. This partially explains outcome differences between high- and low-volume sites.
It has been suggested that a yearly volume of 50 cases is reasonable enough for a single operator. In consequence, since CTOs are present in 20% of all angiographies and only some of them are indicated for treatment, at least 500-600 angiographies are necessary for a single operator to maintain his/her skills.
Taking all of that into account, is rechanneling worth trying?
Studies usually compare patients with successful vs. unsuccessful rechanneling. This represents a huge bias, since patients with successful rechanneling are obviously going to experience higher relief of symptoms and lower mortality rates. None of these studies can answer the question of whether angioplasty is better than optimal medical treatment in this context.
Two randomized studies measured outcomes for chronic total occlusions. On the one hand, the EXPLORE (Evaluating Xience and Left Ventricular Function in Percutaneous Coronary Intervention on Occlusions After ST-Elevation Myocardial Infarction) trial randomized 304 patients initially admitted with acute myocardial infarction, who received primary angioplasty and also presented CTO in a non-culprit vessel.
The primary endpoint was ventricular fraction, which presented no differences between rechanneling and medical treatment. It may only be worth it in cases in which total occlusion is present in the anterior descending artery.
The second randomized study was DECISION-CTO (Optimal Medical Therapy With or Without Stenting for Coronary Chronic Total Occlusion), which enrolled 834 patients to undergo rechanneling or medical treatment. Despite a 91% rechanneling success rate, no differences were observed between groups at 3 years. This study was criticized for its early finalization due to slow enrollment, its 20% rate of crossover from medical treatment to rechanneling attempt, and strong doubts on whether CTO was actually the culprit lesion.
Collectively, these works failed to justify routine rechanneling for all CTOs, which opens the door to opinions on how these must be considered for medical treatment only (particularly if present in a single vessel, with moderate symptoms, or low ischemic value).
The following recommendations could be offered:
- Rechanneling should only be attempted in high-volume sites in which cardiac surgery is available.
- Rechanneling should only be performed by expert, CTO-dedicated operators. No more than two operators per site are necessary.
- Patients selected for CTO should present documented ischemia and significant symptoms in spite of medical treatment optimization. The COURAGE study suggested an ischemic value of over 10% as indication that the procedure is worth trying. The ISCHEMIA study will surely provide more information on that matter.
Original title: Percutaneous Revascularization of Chronic Total Coronary Occlusion. For Whom?
Reference: Andrew Kei-Yan Ng et al. Circ Cardiovasc Interv. 2017;10:e005512.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology
We are interested in your opinion. Please, leave your comments, thoughts, questions, etc., below. They will be most welcome.