Percutaneous coronary interventions have improved during the last decade with 15% rate of target vessel failure (TVF) at 5 years according to the latest reports. We are already familiar with the benefits of functional assessment of lesions with FFR and its clinical outcomes.
Additionally, low post PCI FFR values (FFR ≤ 0.83-≤0.91) have been associated with higher major cardiovascular events (MACE) rate. Some observational studies have shown that post PCI FFR values might increase when adding a stent or with post dilation. However, these studies were not designed to and have no power to identify such increase.
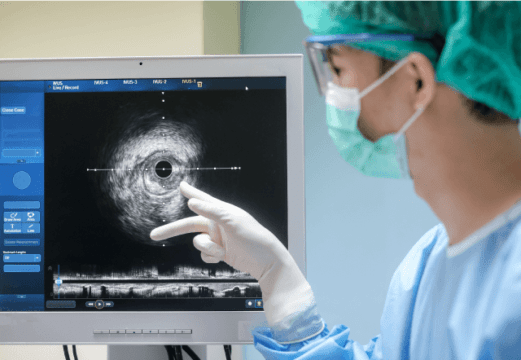
The aim of this randomized single center study was to assess whether PCI optimization guided by intravascular ultrasound (IVUS) in patients with post-PCI FFR <0.90 could improve 1-year TVF rates vs standard medical care.
Primary end point was TVF at one year defined as a composite of cardiac death, target vessel MI, and clinically driven target vessel revascularization. Secondary end point was all cause mortality, AMI, revascularization, MACE, stroke, and stent thrombosis.
291 patients with FFR < 0.90 were randomized: 145 received IVUS guided optimization and 146 went to the control group. Mean age was 66, and they were mostly men. The most frequent clinical presentation was stable angina. The anterior descending artery was the most treated vessel, and B2/C coronary lesion was the most frequent in the IVUS group, resulting in more and longer stents. Mean post PCI FFR was 0.84 ±0.05.
In the IVUS group, stent subexpansion was found in 62% of vessels, while residual focal lesions were 14% proximal and 16% distal. Only 9% of vessels met stent optimization criteria according to the ULTIMATE study.
In the IVUS group, 68% of vessels required additional treatment, 33% requiring post dilation only (scenario 1), and 34% requiring an additional stent, 16% with no post-dilation (scenario 2) and 18% an additional stent and optimization with post-dilation (scenario 3). Of the vessels requiring an additional stent, 19% were distal, 11% proximal and 3% both.
Mean post PCI FFR in the IVUS group increased significantly after additional treatment (0.82 ±0.06 to 0.85 ± 0.05, P< 0.001), significantly higher than in the control group. After optimization, 20% presented FFR > 0.90. Final FFR increased significantly in the three scenarios, but the biggest increase was seen in the group with an additional stent (P=0.011). The IVUS group showed stent implantation resulted in increased minimal lumen area vs. unstented vessels. (P<0.05).
Procedural time, contrast amount and fluoroscopy time was higher in the IVUS group.
There were no differences in primary end point with TVF at one year, which was 4.2% in the IVUS group vs 4.8% in the control group (P=0.79). There was a tendency towards lower clinically driven TVR in the IVUS group (0.7% vs 4.2% P= 0.06). Finally, there was no TVF with post PCI FFR >0.90 after optimization.
Conclusion
Despite this study’s lack of statistical power, IVUS guided optimization post-PCI FFR <0.90 did not affect TVF at one year vs. standard care. Physiological outcomes and lumen area did increase, but with no correlation with a clinical benefit.
Dr. Andrés Rodríguez.
Member of the editorial board of SOLACI.org.
Original Title: FFR-Guided PCI Optimization Directed by High-Definition IVUS Versus Standard of Care. The FFR REACT Trial.
Reference: Tara Neleman et al J Am Coll Cardiol Intv 2022;15:1595–1607.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





