Transradial access is the preferred route in most coronary procedures due to its proven reduction in mortality compared to transfemoral access. However, one of its most frequent—albeit usually silent—complications is radial artery occlusion (RAO).
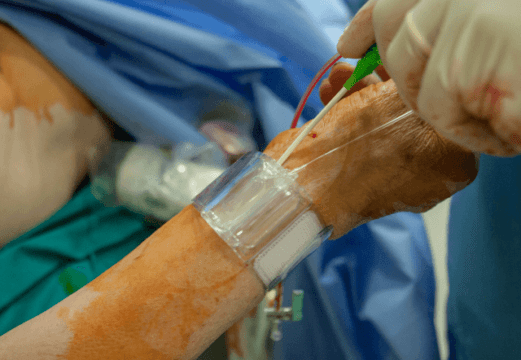
Preventing RAO is essential to preserve future vascular access, thus keeping surgical options, such as grafts or fistulas, available. In this context, distal transradial access (dTRA) has gained popularity, as has the use of periprocedural anticoagulation (AC), although comparative evidence remains limited to small patient reports.
The aim of the study presented by Stiermaier et al., from University Heart Center Lübeck (Germany), was to assess—through a 2×2 factorial design—whether dTRA and periprocedural anticoagulation can reduce the incidence of RAO and bleeding events in patients undergoing diagnostic coronary angiography (CAG).
The RAPID study was a randomized, single-center, open-label trial comparing dTRA vs. cTRA (conventional transradial access) and AC vs no AC in 439 patients undergoing diagnostic CAG. Patients with an indication for percutaneous coronary intervention (PCI) during the index event, known RAO, or a radial artery that was difficult to palpate were excluded. The primary endpoint (PEP) was the presence of RAO (as assessed by Doppler ultrasound) and bleeding (classified by BARC criteria).
The analyzed population included 439 patients; the average age was 73 years, 56.7% of patients were men, and 36.9% were on oral anticoagulant therapy. Right transradial access was the most commonly used alternative (93%), and intravenous nitroglycerin was administered upstream in 33.4% of cases.
In this cohort, distal access did not reduce the incidence of RAO (20.3% vs 21.2%; p=0.810) or bleeding (4.1% vs 6.9%; p=0.188), but it was associated with a higher rate of puncture failure (11.3% vs. 4.1%), greater need for crossover (14.9% vs. 8.3%), and longer procedure times (25 vs. 20 minutes; p=0.001). Additionally, the subjective pain experience was greater with dTRA.
On the other hand, periprocedural anticoagulation significantly reduced RAO (7.3% vs. 33.9%; p <0.001) without increasing the risk of bleeding (7.3% vs. 3.6%; p=0.087). This benefit was consistent in subgroups with dTRA and in patients on chronic oral anticoagulation. All bleeding events were mild (BARC 1-2).
Conclusions
Systemic anticoagulation during diagnostic CAG significantly reduces the incidence of RAO, even in patients on chronic anticoagulation or with dTRA. In contrast, in this study, distal transradial access did not provide clinical benefits and was associated with longer procedure times.
Original Title: Distal access and procedural anticoagulation to prevent radial artery occlusion after coronary angiography – the randomised RAPID trial.
Reference: Stiermaier T, Grünewälder M, Pätz T, Rawish E, Joost A, Meusel M, et al. Distal access and procedural anticoagulation to prevent radial artery occlusion after coronary angiography: the randomised RAPID trial. EuroIntervention. 2025;21:e366–e375. doi:10.4244/EIJ-D-24-00846.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





