Chronic limb-threatening ischemia in patients without conventional revascularization options represents one of the most challenging scenarios within peripheral arterial disease, with 1-year major amputation rates reaching up to 67%. In this context, transcatheter deep vein arterialization (TADV) has emerged as a potential rescue strategy. The aim of this study was to perform a systematic review and meta-analysis to evaluate the clinical outcomes of TADV compared with standard of care (SoC) in patients with critical limb ischemia who lack revascularization options.
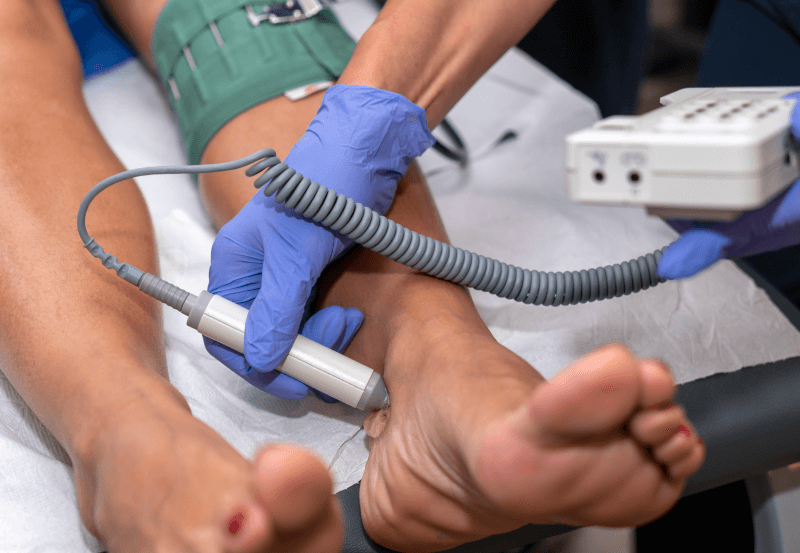
Deep vein arterialization consists of creating a fistula between a tibial artery and the distal venous system of the foot, disabling venous valves and using the venous network as a perfusion pathway to supply ischemic tissues when no distal arteries are suitable for revascularization.
The primary endpoint was limb salvage at 12 months (freedom from major amputation above the ankle). Secondary endpoints included technical success, amputation-free survival, overall survival, wound healing, changes in Rutherford classification, and need for reintervention.
The analysis included four multicenter TADV studies (PROMISE I, PROMISE II, PROMISE-UK, and ALPS), comprising 197 patients, compared with 180 patients from the CLariTI registry treated with standard management. Mean age was 68.7 and 68.9 years, and 68.9% and 66.7% were male in the TADV and control groups, respectively. The prevalence of diabetes ranged from 74% to 76%, and approximately 62% had a history of smoking, with no significant differences between groups.
Read also: Transcatheter Paravalvular Leak Closure: Mid-Term Outcomes and Prognostic Factors.
Most patients had advanced disease (Rutherford class 5–6), and 81% had a history of prior endovascular interventions in the affected limb. All included patients were considered “no-option,” meaning they had no suitable arterial targets for bypass or distal angioplasty and had failed or were not candidates for conventional revascularization. Standard treatment consisted primarily of local wound care, infection control, pain management, and amputation when necessary.
12-Month Outcomes of Transcatheter Deep Vein Arterialization: Improved Limb Salvage and Survival
Technical success of the TADV procedure was 97.6% (95% CI 93.8–99.1%). Limb salvage at 12 months was significantly higher with TADV (79.6% vs 55.1%; p < 0.001), as were amputation-free survival (71.0% vs 37.3%; p < 0.001) and overall survival (90.2% vs 66.8%). Wound healing was also superior in the TADV group, with complete or near-complete healing rates ranging from 85% to 100%, compared with 53.2% under standard treatment.
Reinterventions were relatively frequent, particularly during the first months. In PROMISE-UK, 43% of patients required at least one reintervention within the first year, and in PROMISE I and II, multiple additional procedures were reported during follow-up, reflecting the need for repeated interventions to maintain patency of the arterialized circuit.
Patency rates were variable. In PROMISE I, primary patency was 90% at 1 month and 40% at 6 months, while in PROMISE II, primary patency was 25.9%. Despite these figures, the clinical benefit in terms of limb salvage was maintained in many cases, suggesting that the mechanism of action of venous arterialization does not rely exclusively on sustained conduit patency, but also on hemodynamic and microvascular changes induced by the procedure.
Conclusion: TADV vs Standard of Care in “No-Option” Critical Limb Ischemia: Clinical Impact and Reintervention Rates
In summary, transcatheter deep vein arterialization demonstrated a substantial clinical advantage over standard treatment in patients with critical limb ischemia without revascularization options, with higher rates of limb salvage, amputation-free survival, and wound healing. These findings represent a meaningful therapeutic advance for this high-risk population. However, the need for reinterventions, variability in clinical response, and the limited methodological quality of some studies indicate that further research is required to optimize patient selection and improve long-term outcomes.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





