Courtesy of Dr. Carlos Fava.
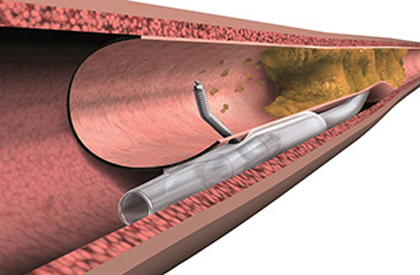 Nowadays, the number of coronary angioplasties carried out on patients with chronic total occlusion (CTO) is increasing due to many studies showing that it improves ventricular function, reduces symptoms, and improves survival. However, most of these works do not include patients of over 75 years old due to their frailty and the presence of comorbidities. In consequence, data available on this population are extremely limited.
Nowadays, the number of coronary angioplasties carried out on patients with chronic total occlusion (CTO) is increasing due to many studies showing that it improves ventricular function, reduces symptoms, and improves survival. However, most of these works do not include patients of over 75 years old due to their frailty and the presence of comorbidities. In consequence, data available on this population are extremely limited.
This study analyzed 2002 patients who underwent angioplasty of a CTO between 2005 and 2013. Among them, 409 (20.4%) were over 75 years old.
In the ≥75 year-old group, most patients were men. They presented higher hypertension, impairment of the left ventricular function, higher rate of myocardial revascularization surgery (MRS), and renal failure. The presence of multivessel lesions was also higher among elderly patients, who also presented higher rates of calcification. Occluded segment length was similar between groups.
The rate of rechanneling success was higher among <75-year-old patients (85.1% vs. 75.1%; p < 0.001), as was the rate of retrograde rechanneling. Fluoroscopy time and procedural time were lower in this population.
The rates of in-hospital major adverse cardiac events (MACE) were similar among groups; 9 patients died (cardiac death in 8 cases; septic shock in 1), and the elderly group required transfusions more commonly (2.2% vs. 0.2%; p < 0.001).
The follow-up was 2.6 years. In total, 238 patients died. All-cause mortality was higher among the elderly (26.7% vs. 8.3%; p <0,001). The rate of MACE was higher among <75-year-old patients (39.6% vs. 28.6%; p < 0.001), as was the incidence of a composite of all-cause death, acute myocardial infarction, and target-lesion revascularization.
The adjusted incidence of MACE was similar for both groups (adjusted hazard ratio [HR]: 1.15; 95% confidence interval [CI]: 0.93-1.41; p = 0.19).
The absolute reduction of all-cause mortality after successful rechanneling was numerically lower for the elderly group. Once variables were adjusted, survival improved for both groups (≥75-year-old HR: 0.58; 95% CI: 0.39-0.87; p = 0.009, vs. <75-year-old HR: 0.59; 95% CI: 0.40-0.86; p = 0.006).
Conclusion
In the era of drug-eluting stents (DES), successful angioplasty of a CTO in patients who are ≥75 years old derives a survival benefit similar to that obtained by younger patients. These findings suggest that CTO angioplasty, when indicated, should not be avoided in elderly patients.
Editorial Comment
This analysis shows that CTOs in elderly patients should be treated, since that reduces the rate of mortality, a hard event. However, such treatment poses a great challenge, since this population often experiences more comorbidities than other patients. In this sense, a high level of expertise is important to lower the rates of procedure-related complications.
The use of a transradial approach may surely reduce the need for a transfusion among patients in this group.
It should be emphasized that procedural success for this series improved over time, which shows a learning curve towards these results.
Courtesy of Dr. Carlos Fava.
Original Title: Survival after percutaneous coronary intervention for chronic total occlusion in elderly patients.
Reference: Aurel Toma, et al. EuroIntervention 2017;13:e28-e235.
Get the latest scientific articles on interventional cardiologySubscribe to our weekly newsletter
We are interested in your opinion. Please, leave your comments, thoughts, questions, etc., below. They will be most welcome.





