Dual antiplatelet therapy with aspirin and a P2Y12 inhibitor is the treatment of choice for patients with acute coronary syndrome who undergo coronary angioplasty. Different oral P2Y12 inhibitors (clopidogrel, prasugrel, ticagrelor) present different characteristics as regards efficacy, risk for bleeding, cost, and timing of administration. In this sense, physicians frequently switch among drugs according to the specific clinical scenario.
The recent introduction of an intravenous P2Y12 inhibitor (cangrelor) further adds to the possibilities for switching, although this drug has not arrived in the field of clinical practice yet.
Read also: “Angioplasty Complexity May Define the Duration of Dual Antiplatelet Therapy”.
This expert consensus provides an overview of the pharmacokinetics and pharmacodynamics of these drugs, as well as recommendations for switching between inhibitors according to the clinical scenario.
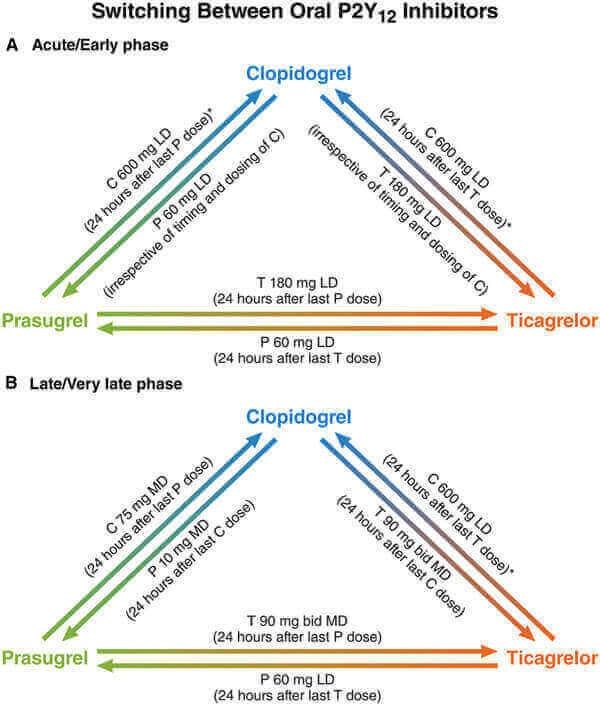
In the acute phase (within 30 days from the index event), a loading dose should be administered in most cases, with the exception of patients who are de-escalating therapy because of bleeding or bleeding concerns (e.g., from ticagrelor or prasugrel to clopidogrel). In this case, continuing clopidogrel 75 mg administered directly 24 hours after the last prasugrel or ticagrelor dose seems reasonable.
Escalation from clopidogrel to prasugrel or ticagrelor after a thrombotic event should occur with the use of a 60- or 180-mg loading dose, regardless of the timing of the last dose of clopidogrel.
Read also: “TCT 2017 | SENIOR: DES with a Bioresorbable Polymer and Short Dual Antiplatelet Therapy in Elderly Patients”.
In the late phase (beyond 30 days from the index event), switching should occur with the administration of a maintenance dose 24 hours after the last dose of a given drug, with the exception of patients changing from ticagrelor to prasugrel therapy, for whom a loading dose should be considered.
The use of a clopidogrel 600-mg loading dose should be considered when de-escalating from ticagrelor to clopidogrel beyond 24 hours after the last ticagrelor dose, except for patients in whom de-escalation occurs as a result of bleeding. For these patients, continuing clopidogrel 75 mg beyond 24 hours after the last prasugrel or ticagrelor dose should be considered.
Read also: “Dual antiplatelet therapy discontinuation causes more thrombotic events at 12 months”.
Undoubtedly, clinical scenarios may be varied, but other variables should also be taken into account. Unfortunately, switching from ticagrelor to clopidogrel because the patient cannot afford the drug or has cognitive limitations that hinder the administration of ticagrelor every 12 hours is relatively frequent.
Original title: International Expert Consensus on Switching Platelet P2Y12 Receptor–Inhibiting Therapies.
Reference: Dominick J. Angiolillo et al. Circulation. 2017;136:1955-1975.
Get the latest scientific articles on interventional cardiologySubscribe to our weekly newsletter
We are interested in your opinion. Please, leave your comments, thoughts, questions, etc., below. They will be most welcome.