The importance of assessing coronary artery disease in patients undergoing transcatheter aortic valve replacement (TAVR) is well recognized due to the high prevalence of such pathology in this population. However, in some cases, patients develop coronary artery disease requiring percutaneous revascularization. This need can be worsened by the difficulties encountered when attempting to cannulate the coronary arteries after TAVR, especially in urgent situations such as in the case of acute coronary syndromes.
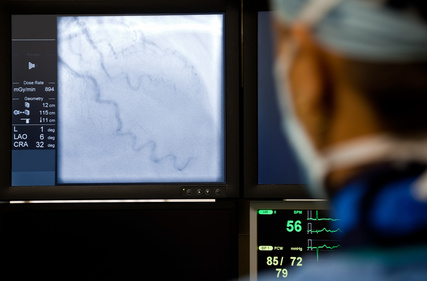
Identifying patients at higher risk of requiring coronary angiography after TAVR could optimize aortic valve replacement management strategies (e.g., prosthesis type selection or surgical preference), improve procedural methods (e.g., coronary access, commissural alignment), and define the ideal timing for revascularization (e.g., percutaneous coronary intervention [PCI] prior to TAVR). This is even more relevant given the increasing indication of TAVR in younger patients with fewer comorbidities, who may require unplanned coronary angiography long after the valve procedure.
The objective of this retrospective study was to assess the incidence, predictors, and clinical outcomes associated with coronary angiography in hospitalized patients who underwent TAVR. A predictive model was also developed to determine the need for subsequent coronary angiography.
The primary endpoint (PEP) was the incidence of unplanned invasive coronary angiography after TAVR, excluding patients for whom the Heart Team had scheduled post-TAVR angiography or PCI, as well as those who underwent an angiography during the procedure.
Read also: Intravascular Lithotripsy in Calcified Coronary Lesions: Success Predictors.
Researchers analyzed a total of 1444 patients. The mean age was 81 years, and most subjects were men. About 6.7% underwent unplanned coronary angiography after TAVR, 45% of them during the first year. The most frequent indication was acute coronary syndrome, in 3.3% of the total. Patients with preexisting coronary artery disease (50.1%) had a significantly higher incidence of unplanned angiography (10.5% vs. 2.9%; p <0.001) compared to the rest of the subjects.
Read also: TAVR Unload: TAVR in Moderate Aortic Stenosis and Ventricular Function Deterioration.
In the multivariate analysis, the following factors were associated with a higher likelihood of unplanned angiography:
- Age >75 years (hazard ratio [HR]: 0.46; 95% confidence interval [CI]: 0.30-0.71; p <0.001)
- Mean aortic valve gradient (HR: 0.82; 95% CI: 0.68-0.98; p = 0.031)
- Dialysis (HR: 2.68; 95% CI: 1.07-6.74; p = 0.036)
- Coronary artery disease (HR: 2.96; 95% CI: 1.76-4.98; p <0.001)
Multivariate models had areas under the curve ranging from 0.71 to 0.77 for predicting unplanned angiography at 5 years.
Conclusion
Approximately 1 in 15 patients undergoing TAVR might require unplanned coronary angiography. Acute coronary syndrome is the most common indication. Comprehensive understanding and management of coronary artery disease in these patients are essential, considering the growing need for lifelong care. The possibility of unplanned angiography should be part of the clinical decision-making process to optimize outcomes.
Original Title: Incidence, Predictors, and Outcomes of Unplanned Coronary Angiography After Transcatheter Aortic Valve Replacement.
Reference: Asa Phichaphop, MD et al JACCCardiovascInterv.2025;18:217–225.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





