Courtesy of Dr. Guillermo Migliaro.
 Events such as very late stent thrombosis and restenosis after first generation DES stenting were associated to the inflammatory response of site implantation. The presence of a durable or permanent polymer was thought to play a central role in said inflammatory process, which caused, among other things, delayed re-endothelialization and neoatherosclerosis.
Events such as very late stent thrombosis and restenosis after first generation DES stenting were associated to the inflammatory response of site implantation. The presence of a durable or permanent polymer was thought to play a central role in said inflammatory process, which caused, among other things, delayed re-endothelialization and neoatherosclerosis.
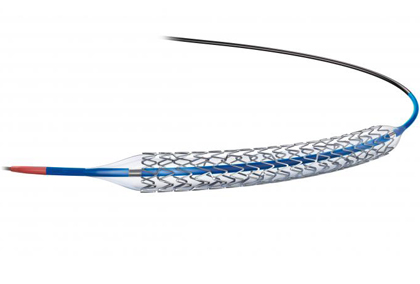
Biodegradable polymer DES have been developed to mitigate this effect by providing, on one hand, the high efficacy of DES, and on the other hand, the safety of conventional bare metal stents.
However, second generation DES with biodegradable polymers have been designed to improve polymer biocompatibility. At present, everolimus eluting stents with cobalt-chromium and platinum-chromium scaffolds, have become the new gold standard given their safety and efficacy profile.
Even though there are randomized studies comparing biolimus and everolimus eluting stents with biodegradable polymers, these lack statistical power to analyze low incidence events separately, such as definite stent thrombosis, death and infarction.
The present study compared the safety and efficacy of biolimus eluting stents with biodegradable polymer (BP-BES) vs. everolimus eluting stents with durable polymer (DP-EES) through a meta-analyzis of the largest randomized studies carried out so far: the NEXT and the COMPARE II trials ( n= 3412 and n=2530), with a total of 5,942 patients.
The study analyzed the following end points at 3 years:
- definite stent thrombosis,
- combined safety endpoint cardiac death or target vessel myocardial infarction
- efficacy endpoint target lesion revascularization
At three-year follow-up, definite stent thrombosis was 0.8% in the BP-BES group vs. 0.4% in the DP-EES group (HR1.71 CI 95% 0.76-3.88 p=0.20), death or target vessel myocardial infarction was 7.8% vs. 6.7% (HR 1.22 CI 95% 0.99-1.54 p=0.07), and repeat TLR was 6.4% in both groups p =NS.
Myocardial infarction (MI) was 6.5% in the BP-BES group vs. 5.3% in the DP-EES group (HR 1.35 CI 95% 1.04-1.75 p=0.03) and this was attributed to higher target MI incidence (5.6 vs. 4.5% HR 1.41 CI 95% 1.05-1.89 p=0.02).
Conclusion
The study concludes that BP-BES and DP-EES present similar safety and efficacy profiles. However, BP-BES present higher target vessel MI incidence.
Editorial Comment
This interesting meta-analyzis does not find significant differences between biolimus and everolimus eluting stents with biodegradable polymers. According to researchers, BP-BES do not seem to offer any advantage over DP-EES and are associated with higher target vessel MI rate and a 50% increased incidence of stent thrombosis. This alone does not explain the higher TV MI rate, but it does when combined with the thinner struts characteristic of everolimus eluting scaffolds, and also explains the rest of the differences.
Courtesy of Dr. Guillermo Migliaro. Buenos Aires German Hospital, Argentina.
Original Title: Biolimus-eluting versus everolimus-eluting stents in coronary artery disease: A pooled analysis from the NEXT (Nobori biolimus-eluting versus Xience/Promus everolimus-eluting Stent) and COMPARE II (abluminal biodegradable polymer biolimus-eluting stent versus durable polymer everolimus eluting stent) randomized trials.
Referencia: Vlachojannis G et al. Eurointervention 2017;12-1970-1977.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology
We are interested in your opinion. Please, leave your comments, thoughts, questions, etc., below. They will be most welcome.





