The transradial access is the preferred access site for patients undergoing acute coronary syndrome. Compared to the transfemoral access site, it reduces the risk of all cause death, vascular complications and major bleeding.
 Radial artery occlusion is the most frequent vascular complication associated to this approach, though it rarely results in clinical consequences such as ischemia, given the dual blood supply to the hand from the radial and ulnar arteries. However, radial artery occlusion becomes a problem when the artery is needed for new catheterization, CABG or dialysis.
Radial artery occlusion is the most frequent vascular complication associated to this approach, though it rarely results in clinical consequences such as ischemia, given the dual blood supply to the hand from the radial and ulnar arteries. However, radial artery occlusion becomes a problem when the artery is needed for new catheterization, CABG or dialysis.
A meta-analyzis of 66 studies showed that radial artery occlusion rate is 11% with a 6 Fr sheath vs. 2% with a 5Fr sheath. Occlusion rate dropss from 7.7% to 5.5% a week after procedure thanks to spontaneous recanalization. The same study showed that occlusion rate is lower with PCI than with diagnostic studies (4.5% vs. 8.8%; p<0.001), probably due to routine use of antiplatelets and higher doses of anticoagulants.
Read also: Transradial Access and Early Discharge in Percutaneous Interventions.
With this in mind, SCAI suggests a few pharmacological and non-pharmacological measures to prevent occlusion:
- A 5000 UI dose of unfractionated heparin (both intra-arterial and intravenous) effectively prevents radial occlusion. Bivalirudin has shown a similar effect. In case of morbid obesity, we should consider a 50 UI/kg dosage.
- Spasm prevention with intra-arterial nitroglycerin and a calcium channel blocker, such as verapamil. After procedure and before sheath removal, an additional dose of nitroglycerin reduced the incidence of occlusion, compared against placebo.
- Minimal sheath-to-artery ratio. Assess left and right radial arteries and choose the one with larger diameter.
- Ultrasound guided radial access: it reduces the number of attempts and wall trauma, though most cath labs are far from using it daily.
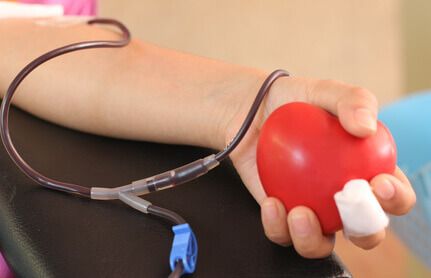
- Compression to get hemostasis but without occluding the artery. Preserving antegrade flow maintaining hemostasis reduces the rate of acute occlusion (12% vs 5%; p<0.05) and occlusion at long term (7% vs 1.8%; p<0.05).
- Consider simultaneous compression of the ulnar artery to improve radial antegrade flow.
- A 30-minute compression for diagnostic studies and 90 to 120-minute compressions in therapeutic procedures is enough to get hemostasis.
Conclusion
The most important maneuvers to keep artery patency after catheterization are: periprocedural anticoagulation, reducing compression time as much as possible, using the smallest sheath size possible, and using the hemostasis technique maintaining antegrade flow.
Título original: Radial Artery Occlusion After Transradial Cardiac Catheterization: Tips on Prevention and Management.
Referencia: Sridevi R. Pitta et al. SCAI’s January 2018 Quality Improvement Toolkit (QIT) Tip.
Get the latest scientific articles on interventional cardiologySubscribe to our weekly newsletter
We are interested in your opinion. Please, leave your comments, thoughts, questions, etc., below. They will be most welcome.





