Peripheral vascular disease (PVD) has been under-studied and under-recognized in comparison with ischemic heart disease and stroke, despite its well-known impact on quality of life and its associated morbidity and mortality. According to a systematic review, it was estimated that in 2015 about 238 million people globally had PVD. This number is on the rise.
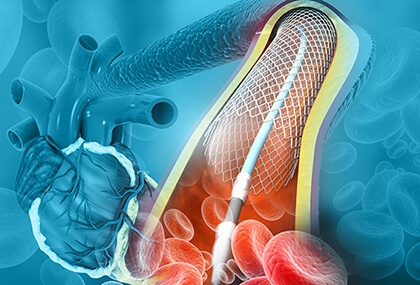
Percutaneous treatment of infrapopliteal disease has shown benefit. However, the best alternative (balloon angioplasty, drug-eluting balloon or conventional/drug-eluting stent implantation) is still unclear, so ongoing research is currently focusing on finding an answer to that question.
The aim of this work, recently published in the Journal of the Society for Cardiovascular Angiography & Interventions, was to perform a systematic review and meta-analysis of randomized studies to evaluate the efficacy and safety of drug-eluting stent (DES) implantation (everolimus/sirolimus/paclitaxel) compared with a control group of endovascular revascularization (plain old balloon angioplasty, drug-coated balloon, stent), for infrapopliteal disease. The primary outcome (PO) was primary patency and the secondary outcomes (SO) were target lesion revascularization (TLR), major limb amputation, and all-cause mortality.
Researchers included 9 randomized studies published in 2007 or after, with a total of 945 patients, whose age range was between 68 and 75 years; most patients were men, with a prevalence of diabetes of 50 to 82%. Follow-up was between a minimum of 6 months and a maximum of 48 months, and, in general, invasive angiography was the method used to assess patency.
Patients treated with DES had a significant increase in primary patency compared with the control group (hazard ratio [HR]: 2.58, 95% confidence interval [CI]: 1.49-4.49; p = 0.0008). When analyzing the SOs, a significant reduction in TLR (HR: 0.48, 95% CI: 0.33-0.68; p <0.0001) was observed, without significant differences in major limb amputation (HR: 0.87, 95% CI: 0.56-1.36; p = 0.28) or all-cause mortality (HR: 0.64, 95% CI: 0.40-1.04; p = 0.95).
Conclusions
The results of this meta-analysis showed better primary patency and lower TLR in patients who underwent infrapopliteal angioplasty with DES compared with conventional revascularization. This benefit in favor of DES use is a similar effect to what was previously observed regarding coronary disease.
Previously, stent revascularization was only reserved as a bailout strategy after balloon angioplasty. This systematic review has some limitations due to the heterogeneity of the studies included and the small number of patients. Based on these results, should we consider the evidence as sufficient to trigger a change in the paradigm for revascularization in infrapopliteal disease?

Dr. Omar Tupayachi.
Member of the Editorial Board of SOLACI.org.
Original Title: Drug-Eluting Stents Versus Conventional Endovascular Therapies in Symptomatic Infrapopliteal Peripheral Artery Disease: A Meta-analysis.
Source: Changal, Khalid et al. Drug-Eluting Stents Versus Conventional Endovascular Therapies in Symptomatic Infrapopliteal Peripheral Artery Disease: A Meta-analysis. Journal of the Society for Cardiovascular Angiography & Interventions, Volume 1, Issue 2, 100024. https://doi.org/10.1016/j.jscai.2022.100024.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





