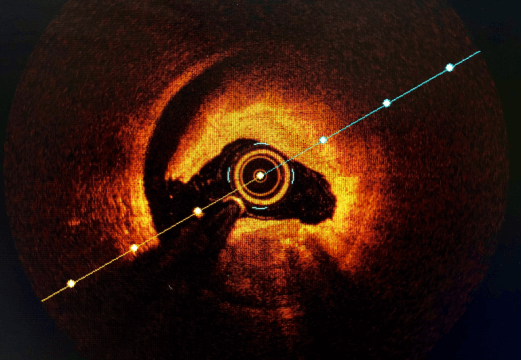
Spontaneous coronary artery dissection (SCAD) is a non-traumatic nor iatrogenic event that causes a separation of the coronary artery tissue due to an intimal tear or a mural spontaneous hemorrhage.
This event is most frequent in young females and usually causes an acute myocardial infarction that could be major.
It accounts for 1% to 4% of all acute coronary syndromes (ACS), and there are no randomized trials on how to address it. We only have different registries and consensus on its treatment.
Researchers conducted an analysis of the prospective CANSCAD registry, which included 750 consecutive patients.
Mean age was 51 years old, 88% of subjects were female, BMI was 26, 4.7% of patients had diabetes, 32% had hypertension, 6% had suffered a prior infarction, 1.7% had undergone prior revascularization, 2.8% had atrial fibrillation, 11% had hypothyroidism, and 32% had migraine.
The incidence of muscular fibrodysplasia was 33%; emotional stress, 50%; inflammatory diseases, 4%; genetic diseases, 1.6%; peripartum state, 4.5%, and connective tissue diseases, 2.9%.
The most frequent clinical presentation was non-ST-segment elevation acute myocardial infarction (68.3%), followed by ST-segment elevation acute myocardial infarction (31.1%) and unstable angina (less frequently).
The most frequent symptom was angina (91%), and 8.3% of patients experienced ventricular tachycardia or ventricular fibrillation. The left ventricular ejection fraction was 55%. In addition, in 25% of patients it was <50%, and 4% of patients experienced alterations in parietal motility.
The dissection was most frequent in the anterior descending artery (52.1%), followed by the circumflex artery (37.7%), the right coronary artery (23.2%), and the left main coronary artery (1.5%).
The treatment was conservative in most cases: only 14.1% of patients underwent coronary angioplasty and 0.7%, myocardial revascularization surgery.
The mean hospital stay was 4 days.
In-hospital mortality was 0.1%, and reinfarction was 4.4%. There was no difference in major adverse cardiac events (MACE) between those who received conservative treatment and those who underwent coronary angioplasty.
Read also: Patients with INOCA in the ISCHEMIA Trial.
At the 3-year follow-up, mortality was 0.8%; recurrent acute myocardial infarction, 9.9%, and MACE, 14%.
The treatment at 3 years was aspirin and beta-blockers in 80% of patients.
Predictors of MACE were genetic diseases, peripartum status, and extracardiac muscular fibrodysplasia.
Conclusion
Long-term mortality in de novo coronary dissections is low in this large contemporary cohort that included a low rate of revascularizations and high use of aspirin and beta-blockers. Genetic disorders, extracoronary muscular fibrodysplasia, and the peripartum period were independent predictors of spontaneous coronary artery dissection in the long term.

Dr. Carlos Fava.
Member of the Editorial Board of SOLACI.org.
Original Title: Canadian Spontaneous Coronary Artery Dissection Cohort Study 3-Year Outcomes.
Reference: Jacqueline Saw, et al. J Am Coll Cardiol 2022;80:1585–1597.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





