The incidence of in-stent restenosis (ISR) requiring repeat revascularization ranges between 5% and 10% of PCI patients receiving new generation drug eluting stents (DES). This is why the current European guidelines on myocardial revascularization recommend treating ISR with drug coated balloons (DCB) with class I recommendation, level of evidence A. DCB are mostly coated with paclitaxel because of its tissue absorption and vessel retention capabilities. One of these devices, the Dissolve DCB, a new generation device, presents paclitaxel associated with medium chain triglyceride as excipient.
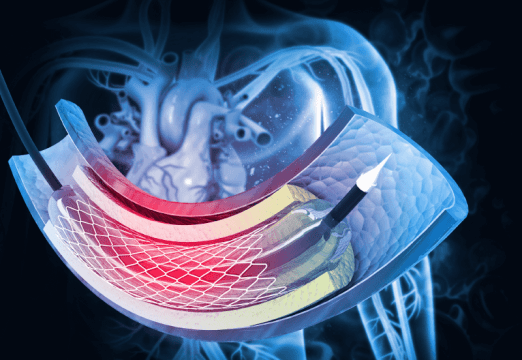
The aim of this multicenter, retrospective, randomized study was to compare the Dissolve DCB against the SeQuent Please DCB (paclitaxel coated balloon associated to a Iopromide as hydrophilic excipient) on angiographic efficacy and clinical outcomes in ISR patients.
Primary end point was late lumen loss (LLL) at 9 months. Secondary end point was acute events rate, restenosis at 9 months, target lesion failure (TLF), target lesion revascularization(TLR), and target vessel failure (TVF). In addition, they assessed a composite of major adverse cardiovascular events (MACE) defined by all cause death, AMI, stroke and all revascularizations.
260 ISR patients were randomized to Dissolve DCB (N=128) and SeQuent Please DCB (N=132). Mean age was 62 and most patients were men. There were no differences between the groups as regards cardiovascular risk factors and prior adverse events. There was a significant difference in post procedural stenosis percentage, which resulted significantly higher in the Dissolve DCB (P=0.006) group.
As regards outcomes, there were no significant differences between the groups when it came to primary end point (Dissolve DCB 0.50 – 0.06 mm vs SeQuent Please DCB 0.47 – 0.07 mm, 0.02 mm difference; CI 95%: 0.13 to 0.18 mm) with Dissolve DCB reaching non-inferiority (P=0.03). There was more restenosis in the Dissolve DCB group compared against the SeQuent Please DCB, but with no statistical significance (P= 0.19).
Read also: Drug-Eluting Balloon in STEACS: Leaving No Trace is Beneficial?
As regards primary end point, TLR and TLF rates, there were no statistical significant differences between the groups. However, TVR at 9 months was significantly higher at the expense of the Dissolve DCB (P=0.02). There were no differences in MACE.
Conclusion
The new Dissolve DCB resulted non-inferior to the SeQuent Please DCB in late lumen loss. However, this new device presented increase TLF and restenosis, which calls for clinical long term follow up.
Dr. Andrés Rodríguez.
Member of the Editorial Board of SOLACI.org.
Original Title: A Randomized Comparison of 2 Different Drug-Coated Balloons for In-Stent Restenosis.
Reference: Shengwen Liu, MD et al J Am Coll Cardiol Intv 2023;16:759–767.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





