The antegrade dissection and re-entry (ADR) technique is considered essential for the management of chronic total occlusions (CTO). It serves as the primary option in some protocols for complex and extensive lesions or as a backup strategy in case of failure with other initial strategies.
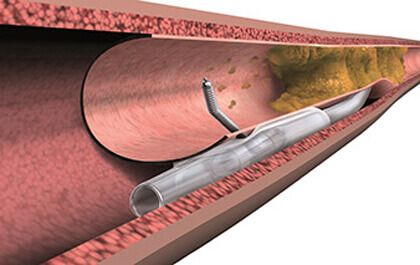
Dissection techniques include guided methods such as scratch and go, balloon-assisted subintimal entry (the BASE technique), the side BASE technique, the Carlino technique, and device-based strategies like Crossboss. For vessel re-entry, the guide-based methods include subintimal tracking and reentry (the STAR technique) and limited subintimal tracking (the LAST technique), as well as specific devices such as the Stingray System.
The aim of this study was to assess the frequency and outcomes of ADRs performed in the PROGRESS-CTO registry. Researchers analyzed the characteristics of patients from 46 centers, evaluating technical success (less than 30% residual stenosis) and procedural success (technical success without in-hospital major adverse cardiovascular events [MACE]).
The Registry collected data from 12,568 patients with 12,841 CTOs between 2012 and 2023. ADR was used in 18.6% of cases, with a trend to decrease over time. Patients undergoing ADR were mostly older men with dyslipidemia, peripheral arterial disease, and a family history of coronary artery disease/angioplasty or coronary bypass.
Read also: MYVAL, a TAVR Balloon-Expandable Valve with Promising Results.
ADR was chosen as the primary strategy in 17.9% of cases, as the secondary strategy in 61.3% of cases, and as a tertiary strategy in 20.8% of subjects. The right coronary artery was the most frequently treated (60.6% vs. 50.4%). Angiographically, lesions were more complex with ADR. ADR was successful in 62% of cases, and rescue with a retrograde approach was required in 45.8% of cases where ADR failed. Additionally, procedure and fluoroscopy times were longer with ADR.
Regarding in-hospital events, technical success was lower with ADR (77.0% vs. 89.3%) and so was procedural success (75.5% vs. 88.1%). Patients who underwent ADR had a higher incidence of MACE (3.7% vs. 1.6%), myocardial infarction (0.92% vs. 0.44%), and pericardiocentesis (2.01% vs. 0.67%), and higher rates of perforation (8.64% vs. 3.81%).
Conclusions
Patients treated with ADR had a higher prevalence of comorbidities and complex lesions, and a higher incidence of MACE compared with patients who received non-ADR strategies.

Dr. Omar Tupayachi.
Member of the Editorial Board of SOLACI.org.
Original Title: Trends and Outcomes of Antegrade Dissection and Re-Entry in Chronic Total Occlusion Percutaneous Coronary Intervention.
Reference: Rempakos, A, Alexandrou, M, Simsek, B. et al. Trends and Outcomes of Antegrade Dissection and Re-Entry in Chronic Total Occlusion Percutaneous Coronary Intervention. J Am Coll Cardiol Intv. 2023 Nov, 16 (22) 2736–2747. https://doi.org/10.1016/j.jcin.2023.09.021.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





