The upfront 2-stent strategy for left main bifurcation treatment presents a technical challenge and has been associated to higher risk of unfavorable outcomes vs provisional stenting. However, the DK-CRUSH technique has been shown to reduce the incidence of adverse events at 3 years. Even though the European Bifurcation Club stands for provisional stenting, 22% of these patients required a second stent.
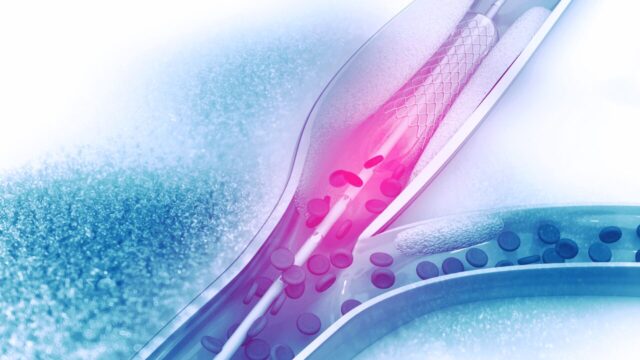
Therefore, defining left main stenting criteria is vital to improve clinical outcomes. To this end, intravascular ultrasound is used for adequate stent expansion and better clinical outcomes.
The aim of this retrospective study was to assess optimal minimal stent area criteria for up-front left main 2-stenting and its long-term clinical outcomes.
Primary end point was major adverse cardiac events at 5 years, including all cause death, acute MI and target lesion revascularization.
Read also: Severe Aortic Stenosis in Bicuspids: Promising Self-Expanding Valve Outcomes at 3 years.
The final analysis included 292 patients, mean age 64, mostly men, most presenting left main and two-vessel disease (55.8%). 6.8% presented acute coronary syndrome. Mean ejection fraction was 60% and 96% presented true angiographic bifurcation, according to Medina classification (1,1,1), (0,1,1) and (1,0,1).
Minimal stent area cutoff values for best predicting major adverse cardiovascular events at 5 years were 11.8 mm² for distal left main (area under the curve, 0.57; P = 0.15), 8.3 mm² for ostial left anterior descending artery (area under the curve, 0.62; P = 0.02) and 5.7 mm² for ostial left circumflex artery (area under the curve, 0.64; P = 0.01).
Read also: Endovascular Management of Chronic TEPH: Is Coronary Management Extrapolatable in This Scenario?
Using these criteria, the risk of major adverse cardiac events at 5 years was significantly associated with stent underexpansion in the ostial left anterior descending artery (HR, 3.14; CI del 95%, 1.23–8.06; P = 0.02) and the ostial left circumflex artery (HR, 2.60; CI del 95%, 1.11–6.07; P = 0.03), but not the distal left main (HR, 0.81; CI del 95%, 0.34–1.91; P = 0.63). Patients with stent underexpansion in both arteries, anterior descending and circumflex, had a significantly higher rate of major adverse cardiac events at 5 years vs. patients with no stenting or with one underexpanded stent in either ostium (P<0.01).
Conclusion
This study has shown that stent underexpasion in the anterior descending ostium and the circumflex was significantly associated with worse outcomes at long term after left main 2-stenting for left main stenosis. Minimal stent area cutoff values proposed in this study might serve was reference for left main stenting optimization.
Original Title: Optimal Minimal Stent Area and Impact of Stent Underexpansion in Left Main Up-Front 2-Stent Strategy.
Reference: Ju Hyeon Kim et al. Circ Cardiovasc Interv. 2024;17:e013006.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





