Supported by robust data, favorably compared against the transfemoral, the transradial approach has consolidated as the safest method for percutaneous intervention, particularly in terms of access-related complications and mortality. Thanks to these advantages, the transradial approach has expanded to non-coronary territories, such as the carotid and peripheral.
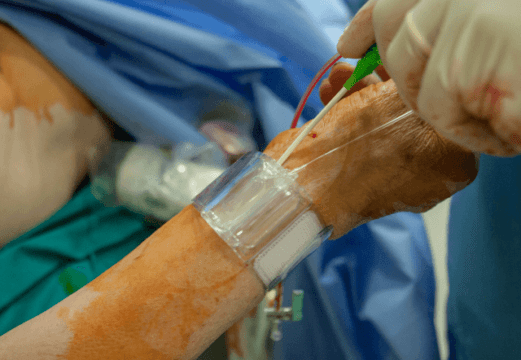
However, it entails challenges such as radial spasm, and radial artery occlusion (RAO) following procedure, which occurs in approximately 9% of cases. The distal radial approach (DRA) has evolved from salvage option for RAO recanalization to preferred access site for transradial procedures, with low occlusion rate due to its excellent anastomotic network.
Objective: Comparative Study of Radial Artery Occlusion between Distal and Traditional Radial Access
The aim of TENDERA (Traditional Entry Point vs. Distal Puncture of Radial Artery), was to compare RAO incidence between DRA and TRA at one-year follow-up. Study operators were required to have experienced at least 100 DRA procedures.
Patients with acute or chronic coronary syndromes (excluding STEMI) were recruited from seven clinical centers in Russia. Those with a history of radial artery interventions, coagulopathies, or ≤1.5 mm radial artery diameter were excluded. Hydrophilic‐coated introducer sheaths (Terumo, Merit, or Lepu Medical) up to 16 cm in length were used for coronary procedures, and access was evaluated prior procedure via ultrasound.
The primary endpoint was Doppler assessed RAO presence. Radial patency was also measured after procedure, at 24 hours and 1, 6, and 12 months. Secondary endpoints included puncture time, time to obtain access, radiation dose (Kerma), major bleeding, and other access-related complications such as hematomas, compartment syndrome, pseudoaneurysm, or fistulas.
Read also: Asymptomatic Aortic Stenosis: A Complex Decision.
In total, 795 patients were included, mean age 63, 66% men. Average wrist circumference was 19.1±2 cm, and 14% of cases were ACS clinical presentations. Mean radial artery diameter was 2.6 mm for the conventional access and 2.27 mm for distal, and 6Fr inductors (82.1%) were mostly used.
Results
RAO incidence resulted 6.7% for the conventional access vs 2.5% for distal (RR 2.59 [CI 95%: 1.29–5.59], p = 0.010). Vascular anomalies were reported in 10.8% of cases, transradial loop being the most common (6.2%). Radial spasm incidence was similar between the groups (23.9% in TRA vs. 23.6% in DRA). However, DRA patients presented higher crossover rate (4.6% vs. 1%, p = 0.013).
Independent RAO predictors included traditional transradial access (OR = 2.59 [CI 95%: 1.29–5.59], p = 0.01), radial/inductor index <1.1:1 (OR = 0.21 [CI 95%: 0.04–0.92], p = 0.048) and female sex (OR = 3.94 [CI 95%: 1.82–8.86], p < 0.001).
Read also: TAVI and Aortic Regurgitation: Are All Valves the Same?
There were no significant differences in total procedural time (20 min [IQR: 8.0–35.0] vs. 20 min [IQR: 10.0–35.0], p = 0.315) or radiation dose (996.9 mGy [IQR: 554.1–1839.1] vs. 924.5 mGy [IQR: 493.1–1709.5], p = 0.238). TRA had a higher incidence of hematomas (27.0% vs. 9.0%, p < 0.001), while only one patient presented pseudoaneurysm.
Conclusions
The TENDERA showed that, with protocolled management, the distal radial access presented a significantly lower incidence of radial occlusion, both in the acute (thrombosis) and late periods (poor vascular remodeling).
Reference: Babunashvili AM, Pancholy S, Zulkarnaev AB, Kaledin AL, Kochanov IN, Korotkih AV, Kartashov DS, Babunashvili MA. Traditional Versus Distal Radial Access for Coronary Diagnostic and Revascularization Procedures: Final Results of the TENDERA Multicenter, Randomized Controlled Study. Catheter Cardiovasc Interv. 2024 Dec;104(7):1396-1405. doi: 10.1002/ccd.31271. Epub 2024 Oct 30. PMID: 39474765; PMCID: PMC11667409.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





