Mitral regurgitation (MR) is a common condition, with approximately 3.5% prevalence in individuals under 65, increasing to 7.7% in those over 75. It can be degenerative (DMR) or functional (FMR).
This condition is associated with left atrial and ventricular dilation, which can lead to arrhythmias, pulmonary hypertension, and heart failure, increasing hospitalizations, worsening quality of life, and raising mortality rates.
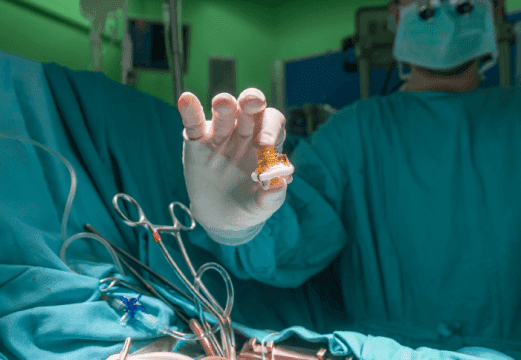
Although surgical repair is the treatment of choice, it is not always feasible, making edge-to-edge treatment (M-TEER) a valid therapeutic strategy.
A total of 136 patients with symptomatic moderate or severe DMR were analyzed; 77 (56.6%) had central MR (A2-P2) while the rest had non-central MR (A1-P1 or A3-P3).
Patient mean age was 69 and 39% being women. Mortality STS was 3.37%. Comorbidities included hypertension in 55%, diabetes in 18%, atrial fibrillation in 31%, coronary artery disease in 37%, COPD in 4%, kidney function deterioration in 12%, prior surgical removal of malignant tumors in 20%, prior CABG in 7%, prior mitral valve surgery in 1%, and prior M-TEER in 1%.
An echocardiogram with Doppler showed, 65% ejection fraction, pulmonary hypertension in 21%, and cardiac damage classification as follows: stage 3 in 12.5%, stage 2 in 40.4%, stage 1 in 37.5%, and the remainder in stage 0. Tricuspid regurgitation ≥2+ was found in 28%, posterior prolapse in 68%, anterior in 24%, and bi-valvular in the rest. There were no significant differences in atrial and ventricular diameters or volumes, nor in the presence of flail or gap.
Read also: New Carotid PCI All-in-One System.
Procedural success rate resulted similar in both groups (93.5% vs. 91.5%, p=0.92), with no differences in need for one or more clips or in residual gradient (3.8 mmHg vs. 3.2 mmHg, p=0.09). Hospital complications were low: mortality 0.74%, SLDA 2.2%, conversion to surgery 2.2%, and pericardial effusion 2.2%.
At one-year follow-up, both groups showed a reduction in ejection fraction, with decreased atrial and ventricular volumes and diameters, maintaining a significant reduction in MR and improving functional class.
At three years, survival free of MR ≤2 was 90.3% among central MR patients and 94.9% for the non-central MR arm (p=0.46).
Read also: Early and Late Outcomes with the ABSORB Bioresorbable Scaffold.
After multivariate analysis, each 1 mmHg increase in gradient was associated with a 36% higher risk of death (HR = 1.36, 95% CI: 1.12–1.66, p = 0.002). Patients with a leaflet-to-annulus index (LAI) ≤1.2 had 3.46 times higher risk of recurrent MR or death compared against those with LAI >1.2 (95% CI: 1.00–11.99, p = 0.05).
Conclusion
M-TEER treatment in non-central DMR showed similar success rate to that of central DMR, with no increase in complications. The seemingly higher success rate in non-central DMR may be due to a lesser impact on the valve area, suggesting the need for further studies to confirm these findings.
Original Title: Comparative Analysis of Central and Noncentral Degenerative Mitral Regurgitation Treated With Transcatheter Mitral Valve Edge‐To‐Edge Repair.
Reference: Peijian Wei, et al. Catheterization and Cardiovascular Interventions, 2025; 105:707–719 https://doi.org/10.1002/ccd.31359.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





