The use of drug-coated balloons (DCB) is emerging as one of the most promising strategies in coronary angioplasty, particularly in clinical scenarios where avoiding permanent stent implantation is desirable.
In a recent position paper by the Academic Research Consortium (ARC), Fezzi et al. provide a comprehensive and up-to-date review of this topic.
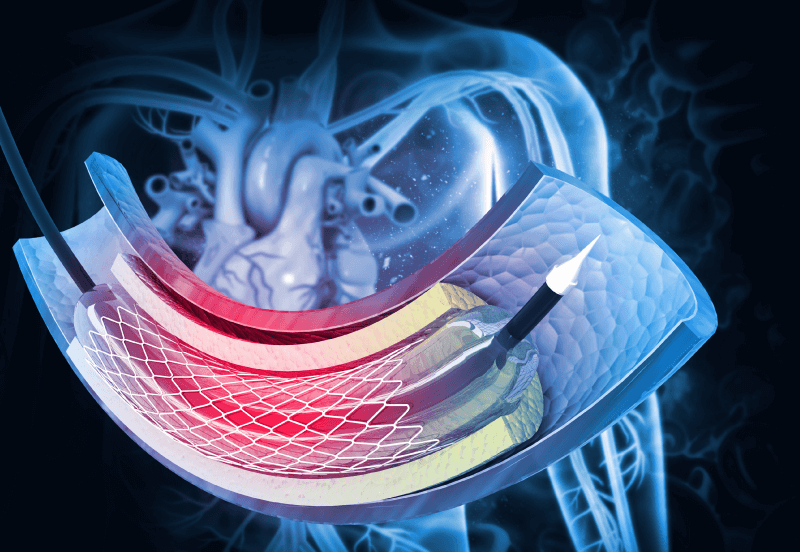
DCBs were designed to locally deliver antiproliferative agents without the need for a metallic scaffold. This approach promotes positive vascular remodeling, preserves physiological vasomotion, and may reduce the need for prolonged dual antiplatelet therapy.
Among the drugs used, paclitaxel has historically been the most common agent due to its high lipophilicity and antiproliferative efficacy. More recently, sirolimus-coated balloons and analogues have been developed, although their bioavailability and long-term effectiveness are still under evaluation.
The document emphasizes that adequate lesion preparation is a critical determinant of procedural success with DCB. Recommended steps include the use of semi-compliant or non-compliant balloons in a 1:1 ratio, prolonged inflations exceeding 30 seconds, cutting balloons for complex lesions, minimizing flow-limiting dissections, and ensuring optimal calcium modification with dedicated devices. The use of intravascular imaging (IVI) is also encouraged to optimize lesion assessment and treatment strategy.
Read also: IVUS Guided PCI: New Expansion Threshold.
The ARC proposes a set of criteria to define an “acceptable” lesion preparation. From an angiographic perspective, residual stenosis should be ≤30% (ideally ≤25% when quantitative angiography is available). The presence of non–flow-limiting dissections—with preserved TIMI 3 flow, no ECG changes, and absence of anginal symptoms—is acceptable and does not contraindicate DCB administration.
Although no standardized IVI optimization criteria exist, the document notes that dissections extending to the medial layer may enhance drug penetration into the vessel wall, according to expert consensus. Similarly, coronary physiology thresholds to guide DCB use after lesion preparation remain undefined.
Clinically, the most established indication for DCBs is in-stent restenosis (ISR), where they have shown superiority over plain old balloon angioplasty and comparable safety outcomes to drug-eluting stents (DES). However, DES still show a slight advantage in reducing repeat revascularizations.
Read also: Use of Drug-Coated Balloons in Chronic Total Occlusions: The ERCTO Registry.
Nevertheless, DCBs are preferable in complex ISR, small vessels, bifurcations, or in the presence of multiple stent layers, as they avoid adding another metallic layer.
Beyond ISR, DCBs have been explored in de novo lesions, particularly in small vessels (<2.75 mm reference diameter), where stent implantation may be technically challenging or undesirable.
In patients at high bleeding risk, DCBs may also allow for shorter dual antiplatelet therapy.
Additional applications include diffuse coronary disease, bifurcations—especially for side branch treatment to prevent jailing and reduce carina shift—and multivessel disease in frail or comorbid patients.
Conclusiones
DCB use in percutaneous coronary intervention represents a valid, safe, and effective alternative across various clinical scenarios, provided that proper lesion preparation and patient selection are ensured.
Although definitive evidence for routine use is still lacking, DCBs may become an essential complementary tool or even a primary “DCB-only” strategy in well-selected contexts, signaling an important evolution in modern interventional cardiology.
Original Title: Indications for Use of Drug-Coated Balloons in Coronary Intervention: Academic Research Consortium Position Statement.
Reference: Fezzi, S, Serruys, P, Cortese, B. et al. Indications for Use of Drug-Coated Balloons in Coronary Intervention: Academic Research Consortium Position Statement. JACC. 2025 Oct, 86 (15) 1170–1202. https://doi.org/10.1016/j.jacc.2025.07.049.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





