
We present the first clinical case in the section “The Fellow’s Corner”, aimed at fellows in Latin America who wish to learn and always be up to date in interventional cardiology.
Leave your thoughts in the comment section of this article and join the conversation!
Case Authors: Jair Suriano Martins (ARG), Leonardo Ripa (ARG).
Moderator: Dr. Nicolas Zaderenko (ARG).
Site: Sanatorio Allende Cerro, Córdoba, Argentina.
Guest Specialist: Dr. José Mangione (BRA). Sao Paulo Beneficencia Portuguesa Hospital.
Case Introduction
DEMOGRAPHICS
- Female
- 55 years old
- Housewife
CURRENT BACKGROUND
- Sedentary lifestyle
- Current tobacco use
- Early menopause (LMP at 38 years old)
REASON FOR CONSULTATION
Chest pain.
CURRENT DISEASE
Consultation in peripheral center due to 30-minute long angina at rest, with peak intensity, which irradiates to an upper limb, is accompanied by neurovegetative symptoms, and changes with respiratory movements.
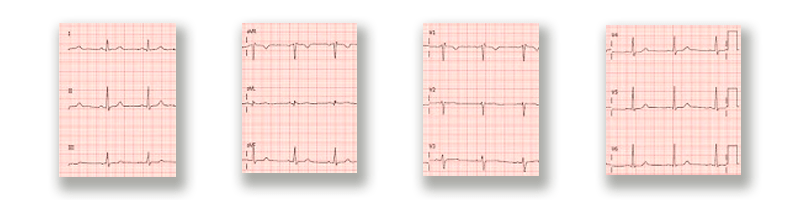
Emergency ECG shows a right branch conduction disorder. Anti-ischemic treatment is conducted and a cardiac enzymes test is requested, which comes back positive (1.3 mcg/mL, NV: < 0.01).
Patient experiences a new angina episode (without electrocardiographic changes) that subsides with nitroglycerin.
Symptomatology is interpreted as high-risk non-ST-segment elevation acute myocardial infarction and the cath lab is activated. An emergency coronary catheterization is performed.
ADDITIONAL STUDIES
ECG
Coronary Angiography
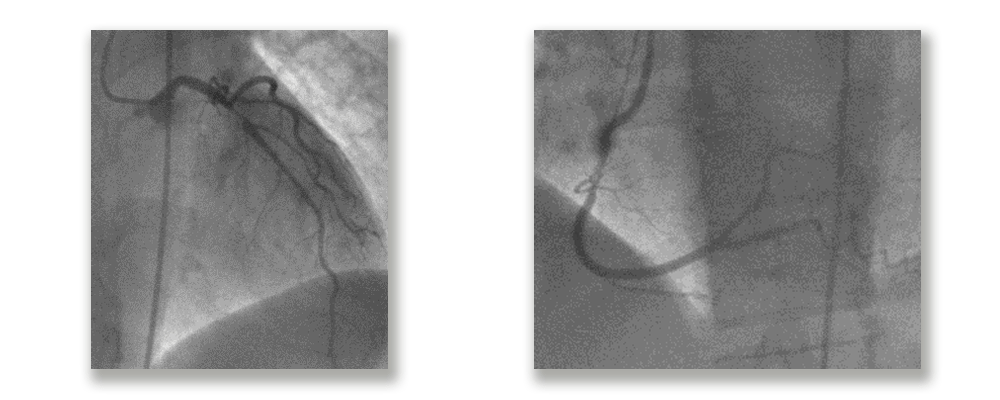
An anterior descending artery lesion is considered as the origin of the event and specialists decide to perform an angioplasty with a 3.0 × 30 mm stent (DES).
DOPPLER ECHOCARDIOGRAPHY
LVEF 58%, LV apical hypokinesis, other parietal motility preserved. Mild LA dilatation. Normal function and contractility RV. Normal Doppler evaluation.
PROGRESS
Patient shows good progression. For administrative reasons, she is referred to our institution to continue her recovery after the infarction and decide whether a complete revascularization should be performed before discharge.
Moderator Comments
Congratulation to Dr Suriano and Dr Ripa of Mendoza Central Hospital for presenting this case.
I believe this is an excellent case to kick-start this discussion forum thought and created for all Latin American fellows.
This is one of the most frequent situations in the cath lab, a patient with a moderate to high-risk non-ST-elevation ACS assessed as an emergency, who has two severe lesions and we need to decide which one to treat. Afterwards, the patient is referred to another site to continue her progress and decide the therapeutic course of action.
Therefore, to start this debate, here are my questions:
- In this case, would you all have treated the LAD?
- What would you take into account to decide the therapeutic course of action?
- Does this case warrant using an invasive or a non-invasive diagnostic method?
- Which would be the therapeutic course of action to follow?
Regards to all!
Dr. Nicolas Zaderenko.
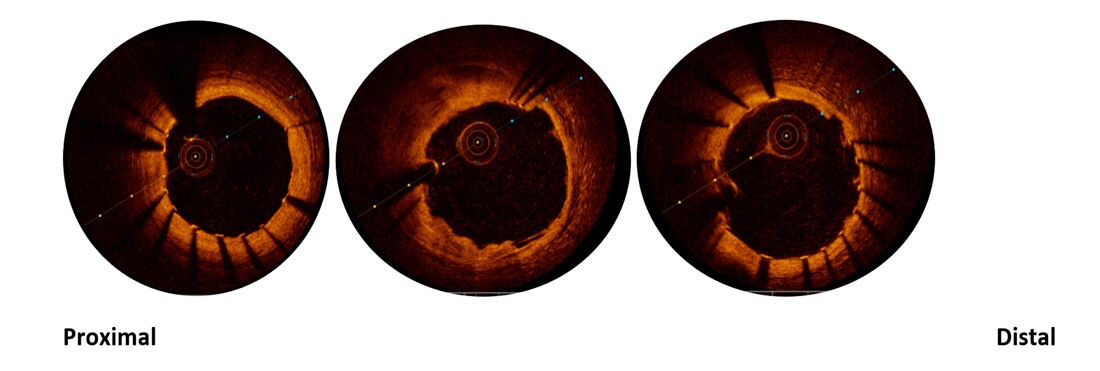
During hospitalization, the case is reassessed with intracoronary imaging following stent implantation in distal left main towards anterior descending, in addition to testing the right coronary.
OCT reveals fibrolipidic plaque in right coronary artery, with erosion and dissection flap, and significant stenosis with thrombus inside.
CD
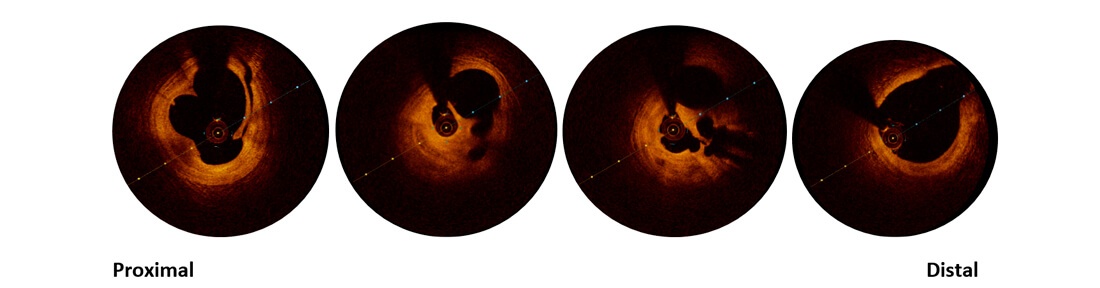
And stent malapposition in descending artery and left main
DA
INTERVENTION
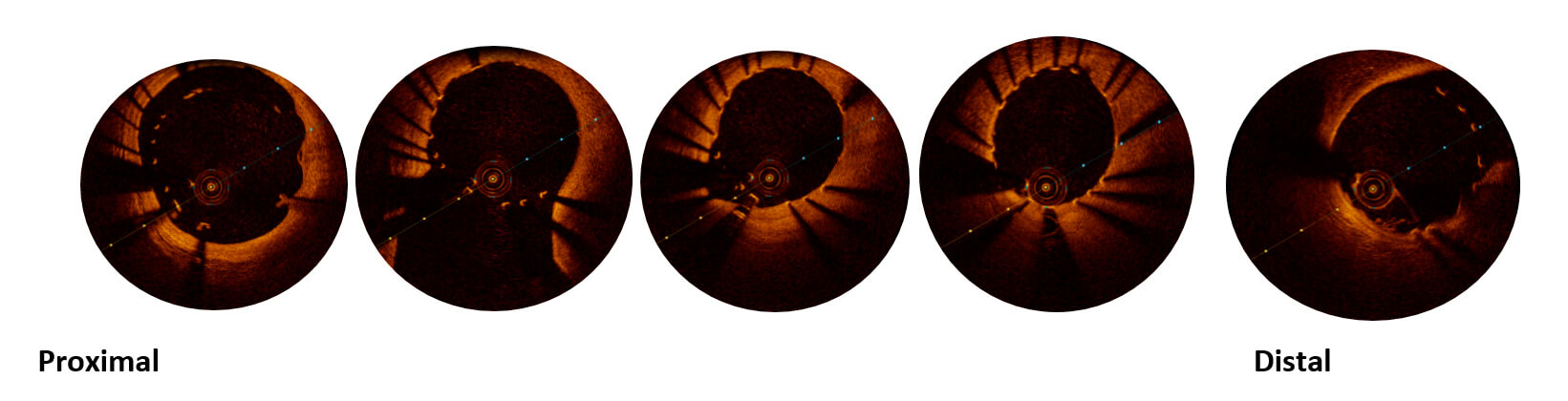
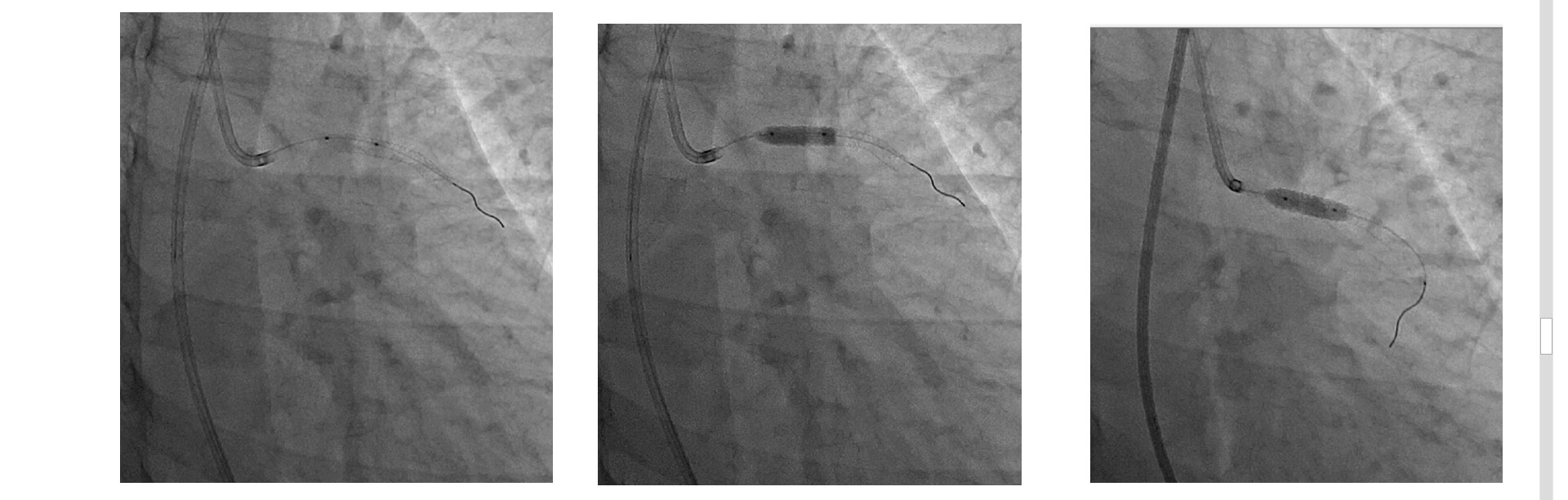
Based on the new imaging, the culprit artery is reinterpreted, the right coronary being the new suspect, which leads to right coronary stenting (video 3 image 3).
CCG

Post OCT
A new strategy is decided, to optimize instent with 3.5x20mm balloon proximal to anterior descending and 4.5mm balloon in middle and distal segment of left main.
Post OCT

EVOLUTION
Asymptomatic at discharge and one-year followup, assessed with non-invasive studies.





