The safety and efficacy of drug-coated balloons (DCB) has been established for the treatment of in-stent restenosis of conventional bare-metal stents (BMS) and drug-eluting stents (DES).
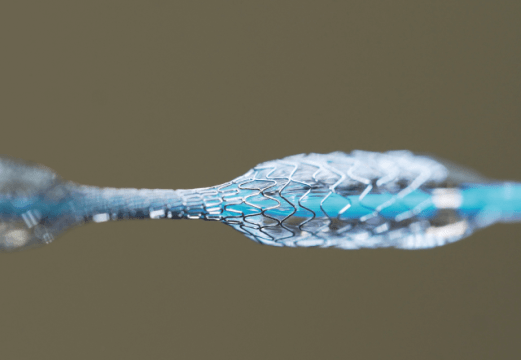
Furthermore, these devices are also used to treat de novo coronary lesions, as demonstrated in the BASKET-SMALL 2—where DCBs were non-inferior to stents—and the DEBUT RCT trials—, where DCBs were superior to BMS in patients at high risk for bleeding.
These patients have a higher risk of bleeding after percutaneous coronary intervention (PCI), which in turn increases their mortality and hospitalization rates. All of this turns choosing an optimal therapeutic plan into a paramount necessity.
The aim of this retrospective study was to evaluate the safety and efficacy of DCB PCI only combined with simple antiplatelet therapy (SAPT).
The primary endpoint (PEP) was major adverse cardiovascular events (MACE) at 12 months, defined as a composite of cardiovascular death, acute myocardial infarction (AMI), and treated lesion revascularization (TLR). The secondary endpoint (SEP) was BARC II-V bleeding, treated vessel revascularization, hospitalization requiring urgency revascularization, stroke, and MACE at 24 months.
Read also: Can Drug Coated Balloon Be a Valid Option for Small Vessels?
This study analyzed 172 patients who received DCB and were discharged to SAPT. Mean patient age was 75 years old, and most subjects were male. At the time of PCI, 65% of patients were anticoagulated.
The most frequent clinical presentation was acute coronary syndrome (ACS, 58%), followed by chronic ischemic heart disease (42%). Most coronary lesions were de novo (96%), with 19% being calcified lesions. The most affected artery was the anterior descending artery, and most treated arteries had a diameter >3mm. Prescribed SAPTs at discharge were aspirin (69.8%) and clopidogrel (21.5%).
In terms of the PEP, the MACE rate at 12 months was low (4.7%). When analyzed, the MACE rate was significantly higher in patients with ACS than in those with chronic artery disease (7.1% vs. 1.4%). All-cause mortality using DCB alone was 4.1% for stable coronary disease and 12.1% for ACS. The TLR rate at 12 months was 0% in stable cardiac conditions and 3% in ACS. There were no treated vessel acute or subacute occlusions.
At 24 months, the MACE rate was 8.1%—significantly higher for ACS when compared with stable coronary disease.
Conclusion
Using DCBs in PCI combined with SAPT was safe with favorable clinical outcomes. This strategy could reduce post-PCI bleeding in patients at high risk for bleeding compared with stent use. This treatment is currently being tested in the DEBATE RCT trial.
Dr. Andrés Rodríguez.
Member of the editorial board of SOLACI.org.
Reference: Alma Räsänen MD et al Catheter Cardiovasc Interv. 2023; 1–10.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





