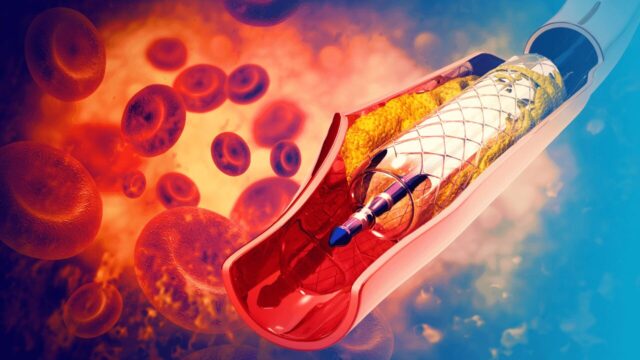
The use of drug-eluting stents and the integration of intravascular imaging techniques have reduced the risk of adverse clinical outcomes following percutaneous coronary intervention (PCI). However, these adverse events can occur through different mechanisms, regardless of whether they are in-stent or stent edge-related.
In the LRP (lipid-rich plaque) and PROSPECT II studies, the use of intravascular ultrasound (IVUS) and the use of near-infrared spectroscopy (NIRS) have shown that the combination of high lipidic content and large plaque volume in untreated non-culprit lesions (NCL) is associated with a higher long-term risk of major adverse cardiac events (MACE). However, the combination of high lipidic content in culprit lesions and large plaque volume, and its effect on outcomes after PCI have not been assessed.
The aim of this PROSPECT II substudy was to assess the importance of lipidic content and plaque volume in the culprit vessel, before and after PCI, using NIRS and IVUS, as well as their relationship with the risk of MACE in the long term in patients with acute myocardial infarction (MI). Additionally, it analyzed whether these events were in-stent or stent edge-related.
The primary endpoint (PEP) was the incidence of MACE in the culprit vessel, defined as a composite of cardiac death, MI, and unstable or progressive angina requiring revascularization.
Read also: Ultrathin vs Thin-Strut Stents in PCI Patients at High Bleeding Risk.
The mean patient age was 64 years, and most subjects were men. The most frequent clinical presentation was non-ST-elevation myocardial infarction (NSTEMI). The most frequently treated artery was the left anterior descending artery, followed by the right coronary artery. During a median follow-up of 3.8 years, researchers assessed 1041 lesions treated with PCI in 768 patients and registered 25 major adverse events related to the culprit vessel: 11 were stent edge-related, 13 were in-stent, and 1 was found in the lesion without a stent.
There was no correlation between lipidic content measurements before or after PCI and in-stent MACE. However, the risk of stent edge-related MACE increased significantly if, after PCI, the lipidic plaque at the stent edge was 4 mm max. and the plaque volume at the edge exceeded 50% (odds ratio [OR]: 4.11 [95% confidence interval (CI): 1.12–15.2]; p=0.03).
Conclusion
In this PROSPECT II substudy, researchers observed that, after IVUS-guided PCI and the use of drug-eluting stents in patients with MI, the rate of MACE related to the culprit vessel was low at 4 years. Lipidic content and plaque volume at the stent edge were identified as the main predictors of stent edge-related MACE, while in-stent lipid-rich plaque was not significantly associated with adverse events.
Original Title: Impact of Lipidic Plaque on In-Stent and Stent Edge–Related Events After PCI in Myocardial Infarction: A PROSPECT II Substudy.
Reference: Lars Kjøller-Hansen MD et al Circ Cardiovasc Interv. 2024;17:e014215.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





