Courtesy of Dr. Leiva.
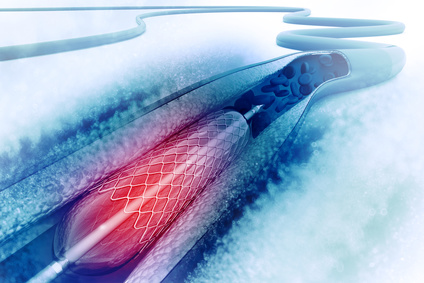
Bioresorbable scaffolds with drug-eluting stents (bioresorbable vascular scaffolds, BVS) have been added to the list of endovascular treatment options for coronary disease. The ABSORB III trial showed the non-inferiority of this stent type to everolimus-eluting metallic stents as regards target-lesion revascularization (TLR) at one year. However, reports have suggested a higher thrombosis risk with bioresorbable scaffolds than with metallic stents.
The Amsterdam Investigator-Initiated Absorb Strategy AllComers Trial (AIDA) is a randomized multicenter study designed to compare both devices in a patient population that reflects that seen in routine clinical practice. While the study was financially supported by Abbott Vascular, the laboratory had no role in the design of the study, the collection or management of the data, or their statistical analysis, nor was it involved in the writing or publication of the manuscript.
The study enrolled patients with coronary disease who were undergoing coronary angioplasty and had one or more target lesions that were considered to be suitable for drug-eluting stent implantation. Exclusion criteria included target lesions more than 70 mm in length, a reference vessel diameter of less than 2.5 mm or more than 4.0 mm, bifurcation lesions (for which the use of two stents was planned beforehand), and in-stent restenosis.
The primary endpoint of target-vessel failure (TVF) was a composite of cardiac death, target-vessel myocardial infarction, or target-vessel revascularization. Secondary endpoints (all-cause death, infarction, all revascularizations, and device thrombosis) were also analyzed.
An analysis was carried out to test whether BVS was noninferior to metallic stents. In November, 2016, the data and safety monitoring board recommended early reporting of the results because of safety concerns.
A total of 1845 patients were enrolled at five high-volume centers in the Netherlands (BVS: 924; bare metal stents: 921); the median duration of follow-up was
707 days.
The results were as follows:
- There was no difference in the primary endpoint (TVF) at 2 years (hazard ratio [HR] BVS: 1.12; 95% confidence interval [CI]: 0.85-1.48; p = 0.43).
- Cardiac death: BVS, 2.0%; bare metal stents, 2.7% (HR: 0.78; 95% CI: 0.42-1.44; p = 0.44).
- Target-vessel myocardial infarction: BVS, 5.5%; bare metal stents, 3.2% (HR: 1.6; 95% CI: 1.01-2.53; p = 0.04).
- No differences in TVR and TLR were observed between groups.
- Event rates of definite or probable thrombosis were 3.5% in the BVS group and 0.9% in the bare metal stent group (HR: 3.87; 95% CI: 1.78-8.43; p < 0.001).
Comments:
In this preliminary report, AIDA trial results show no significant difference at two years between these devices as regards the endpoint. However, the BVS group presented a higher rate of stent thrombosis (3.5 higher than that for bare metal stents), and a significantly higher rate of myocardial infarction.
While the causes of such higher incidence are only partially understood, incomplete lesion coverage, underdeployment, malapposition, or strut thickness could be involved.
As a consequence of these findings, the data and safety monitoring board recommends that dual antiplatelet therapy be extended beyond 1 year for recipients of bioresorbable scaffolds with drug-eluting stents.
Whether changing the way bioresorbable scaffolds with drug-eluting stents are implanted may modify the high adverse event rates observed with this device remains to be seen.
Courtesy of Dr. Leiva.
Original title and reference: Bioresorbable Scaffolds Versus Metallic Stents in Routine PCI. AIDA Investigators. NEJM March 29; 2017.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology
We are interested in your opinion. Please, leave your comments, thoughts, questions, etc., below. They will be most welcome.