Peripheral artery disease (PAD) is no longer a systemic manifestation of atherosclerosis. In fact, 2 in 3 people with PAD have concomitant heart disease, and 1 in 3 people has concomitant PAD.
To understand the real dimension of this problem, we should know that PAD patients have 60% more risk of acute myocardial infarction and between 2 and 6 times higher risk of cardiac death.
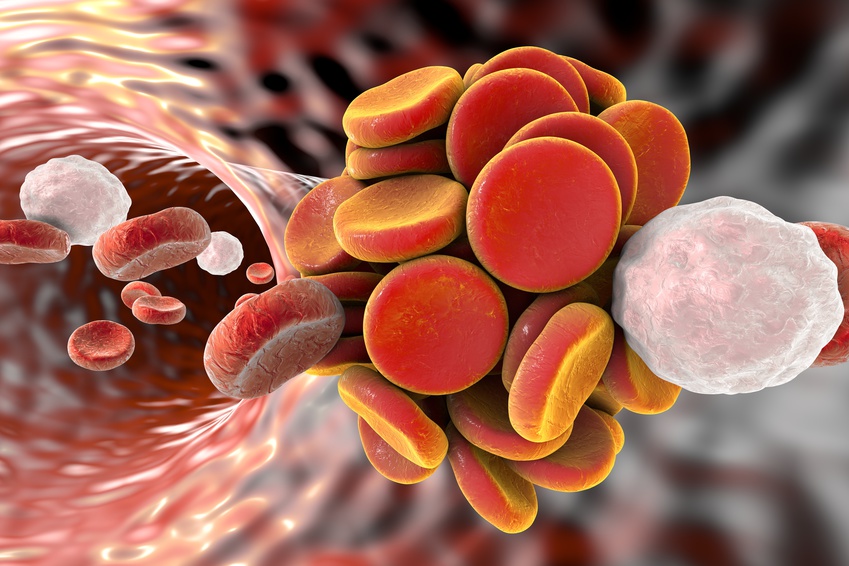
PAD patients undergoing coronary angioplasty procedures present 6 times higher risk of stent thrombosis. Unfortunately, they also present increased bleeding and, in fact, twice the mortality rate.
All the above made us think perhaps PAD diagnosis should change post PCI antiaggregation schemes.
Also read: “Lost Opportunities in Patients with Peripheral Artery Disease”.
This theory was tested in big studies such as the CHARISMA (Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management and Avoidance), where the combination of aspirin and clopidogrel for 28 months v. aspirin alone, reduced infarction rate by 40%, but increased bleeding rate.
The DAPT study (Dual Antiplatelet Therapy) randomized 11648 post coronary angioplasty patients (with no bleeding or ischemic events after one year DAPT) to continue with 18 additional months with aspirin and clopidogrel vs. aspirin alone.
Between months 12 and 30, those with concomitant PAD presented more infarction and thrombosis (6.03% vs. 2.92%; p<0.001), more adverse cardiovascular and cerebrovascular events (11.65% vs. 4.62%; p<0.001) and major bleeding (4.86% vs. 1.74%; p<0.001).
Also read: “Peripheral Artery Disease Associated to Ischemic and Bleeding Events after DES Implantation.”
In this population, those randomized to continue with DAPT were protected against the risk of infarction and thrombosis (HR: 0.63; 95% CI: 0.32 to 1.22) at the cost of more bleeding events (HR, 1.82; 95% CI: 0.87 to 3.83).
Conclusion
Patients undergoing coronary angioplasty that present concomitant PAD have more ischemic and bleeding events than those without PAD.
Editorial Comment
The relationship between peripheral artery disease and adverse events responds to several factors which include elements with increased inflammatory status, disease in multiple territories and concomitant ischemic and bleeding factors, such as advanced age and kidney failure.
Even though peripheral artery disease was associated to more platelet reactivity and less response to antiaggregation, this does not seem to be the case in this study, where both the benefits (reduced thrombosis) and the harm (increased bleeding) resulted similar in patients without PAD.
This is why whether to continue DAPT or not we should assess risks and benefits on a case by case basis, as we do with the general population.
Original Title: Extended Duration Dual Antiplatelet Therapy after Coronary Stenting among Patients with Peripheral Arterial Disease. A Subanalysis of the Dual Antiplatelet Therapy Study.
Reference: Eric A. Secemsky et al. J Am Coll Cardiol Intv 2017;10:942–54.
Get the latest scientific articles on interventional cardiologySubscribe to our weekly newsletter
We are interested in your opinion. Please, leave your comments, thoughts, questions, etc., below. They will be most welcome.