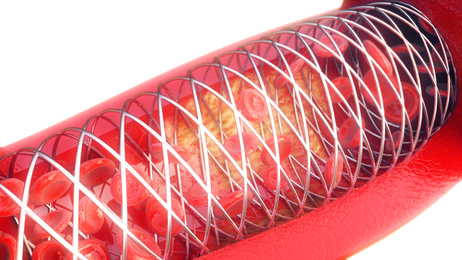
Elective, uncomplicated repeat revascularization after stent restenosis is associated with higher mortality rates according to a new meta-analysis that will be published soon in J Am Coll Cardiol Intrv.
 Historically, interventional cardiologists have seen target lesion revascularization (TLR) as a procedure that “unjustly” increased combined events in clinical studies and our own databases, thus representing a disadvantage for us against surgeons. Many people thought that if patients who underwent TLR did not go into cardiac arrest or die, this event only entailed the nuisance of having to return to the cath lab. This work forces us to start thinking that repeat revascularization is not entirely benign.
Historically, interventional cardiologists have seen target lesion revascularization (TLR) as a procedure that “unjustly” increased combined events in clinical studies and our own databases, thus representing a disadvantage for us against surgeons. Many people thought that if patients who underwent TLR did not go into cardiac arrest or die, this event only entailed the nuisance of having to return to the cath lab. This work forces us to start thinking that repeat revascularization is not entirely benign.
In a pooled analysis of 21 randomized trials that included 32,882 patients, repeat revascularization was an independent predictor of all-cause mortality after adjusting for potential confounding variables (hazard ratio [HR]: 1.23; 95% confidence interval [CI]: 1.04-1.45).
Read also: A mayor nivel de LDL, mayor beneficio en mortalidad con la terapia agresiva.
Even uncomplicated TLR procedures, in which the diagnosis of restenosis resulted from symptoms of effort or a routine study (as opposed to acute coronary syndrome), were still associated with an increased risk of long-term mortality. In that sense, stent restenosis might compete with de novo lesions as regards risk.
In this cohort, 7.2% of patients underwent an elective, uncomplicated target lesion repeat revascularization procedure at a mean of 271 days after the index angioplasty procedure. Comparatively, among the same cohort, 2.5% of patients underwent elective, uncomplicated revascularization of lesions non-related to the one previously treated.
Patients with restenosis were younger, more likely to be female, and more likely to have diabetes and other comorbidities than patients who underwent non-TLR revascularization.
Read also: Revascularización híbrida o cirugía convencional, la historia todavía se está escribiendo.
Mortality among patients who did not require a trip back to the cath lab was 1.87 per 100 patient-years, while among patients with restenosis it was 2.45 per 100 patient-years, and among patients with de novo lesions it was 2.67 per 100 patient-years.
After adjusting for multiple confounders, revascularization due to restenosis was associated with an increased risk of death whereas revascularization of de novo lesions was not.
Patients with restenosis who experienced an acute myocardial infarction sometime during follow-up had a fourfold higher risk of death (HR: 3.82; 95% CI: 2.44-5.99).
Read also: La hipertensión pulmonar basal pre-TAVI no debe contraindicar el procedimiento.
Additionally, researchers excluded from this analysis target lesion revascularizations presented as acute myocardial infarctions and patients who presented peri-procedural infarctions; in consequence, mortality might actually be underestimated.
Perhaps, patients with restenosis are more complex than others (whether from a clinical viewpoint, an anatomical viewpoint, or both), and that is what ultimately contributes to their worse prognosis.
Original title: Mortality Following Non-Emergent, Uncomplicated Target Lesion Revascularization After PCI: An Individual Patient Data Pooled Analysis of 21 Randomized Trials and 32,524 Patients.
Reference: Palmerini T. et al. J Am Coll Cardiol Intrv. 2018; Epub ahead of print.
Get the latest scientific articles on interventional cardiologySubscribe to our weekly newsletter
We are interested in your opinion. Please, leave your comments, thoughts, questions, etc., below. They will be most welcome.





