Here is the third Fellow’s Corner clinical case to keep discussing and learning alongside the entire community of hemodynamics fellows in Latin America.
In this instance, we will present a case of True Bifurcation Lesion: Which Strategy Should We Use?
Authors: Dr. Carlos Fava (ARG) y Franco Andreoli (ARG).
Institution: Fundación Favaloro, Buenos Aires, Argentina.
Moderator: Dr Nicolas Zaderenko (Arg). Sanatorio Allende Cerro, Cordoba, Argentina.
Guest specialist: Dr. Carlos Uribe (COL).
Case Presentation: True Bifurcation Lesion: Which Strategy Should We Use?
- The patient is 43 years old and presents coronary risk factors: smoking and stress.
- They exercise regularly.
- They indicate recent onset angina (New York Heart Association functional class I-II).
- Admission for acute MI, Killip-Kimbal A, progressing for 4 hours.
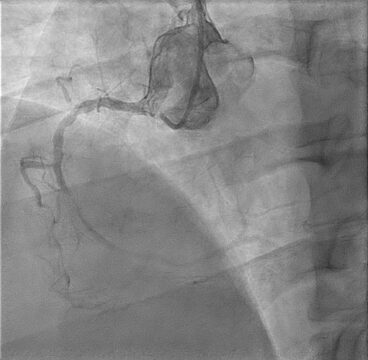
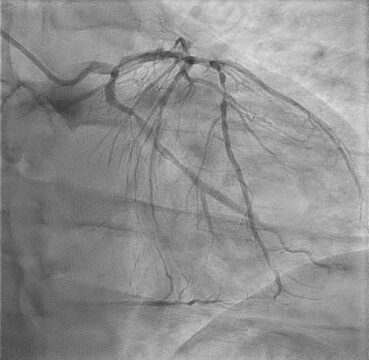
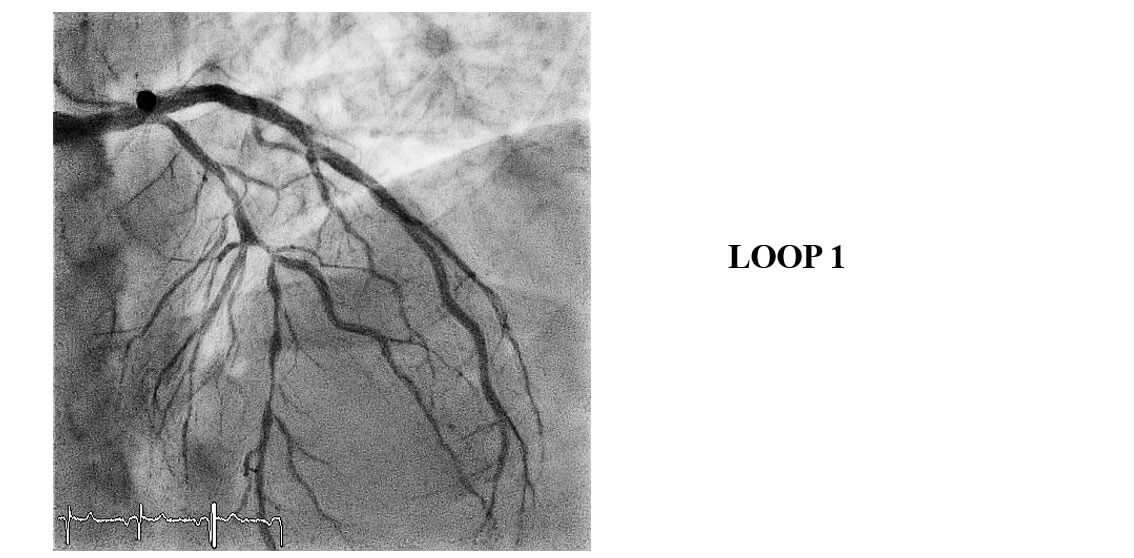
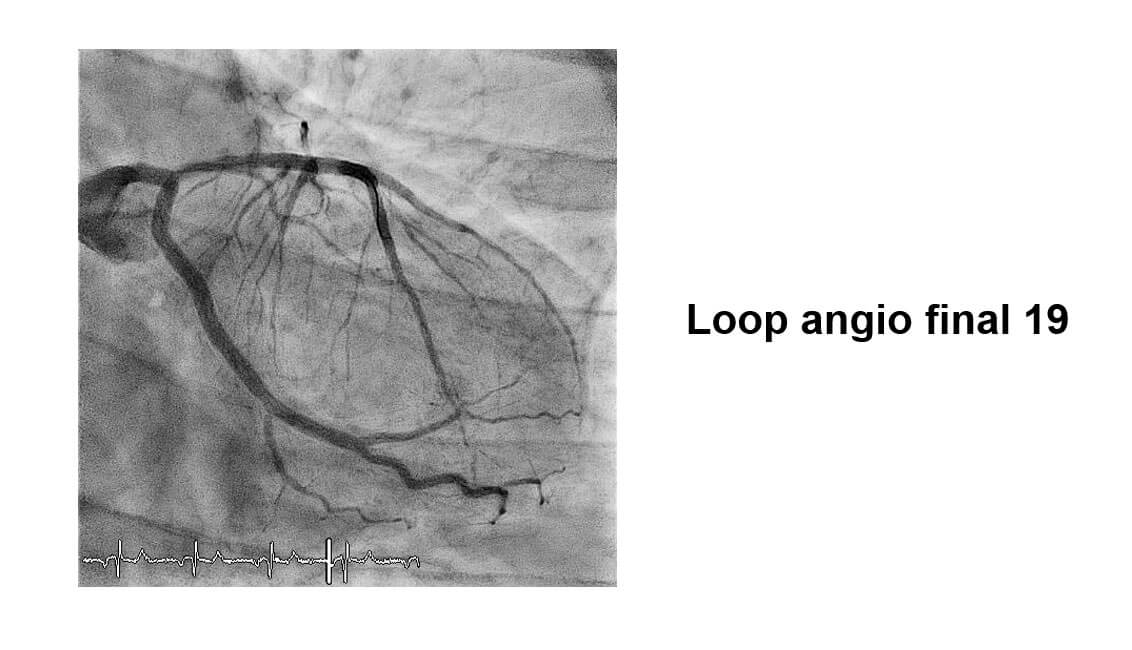
- Coronary angiography was performed. There was evidence of thrombus in the left circumflex artery, an occlusion lesion in the right coronary artery, and a severe long lesion in the anterior descending artery in 1.1.1 bifurcation.
- Primary angioplasty in circumflex artery was performed successfully.
Images from the Case


Case Resolution
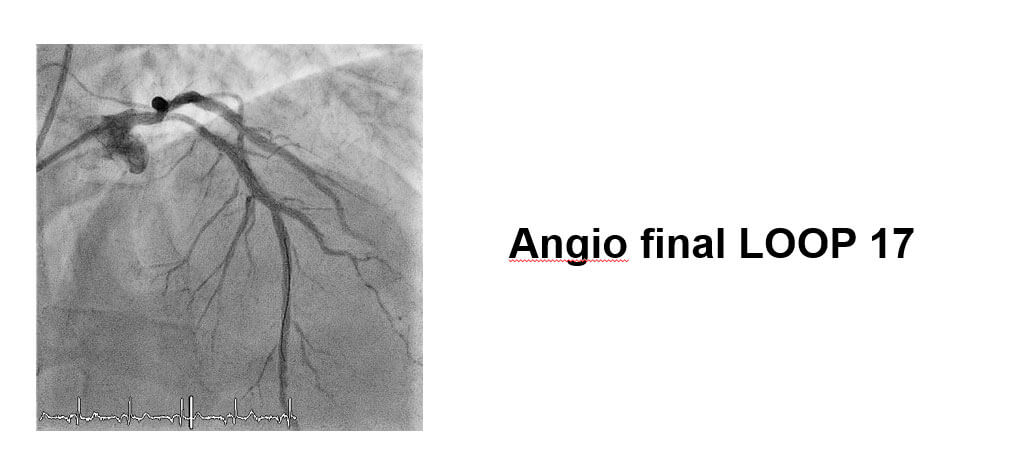
Patient presents good evolution after MI; while hospitalized, after 48 hours, LAD and RCA PCI is decided.
A las 48 horas se decide efectura ATC a CD y DA.
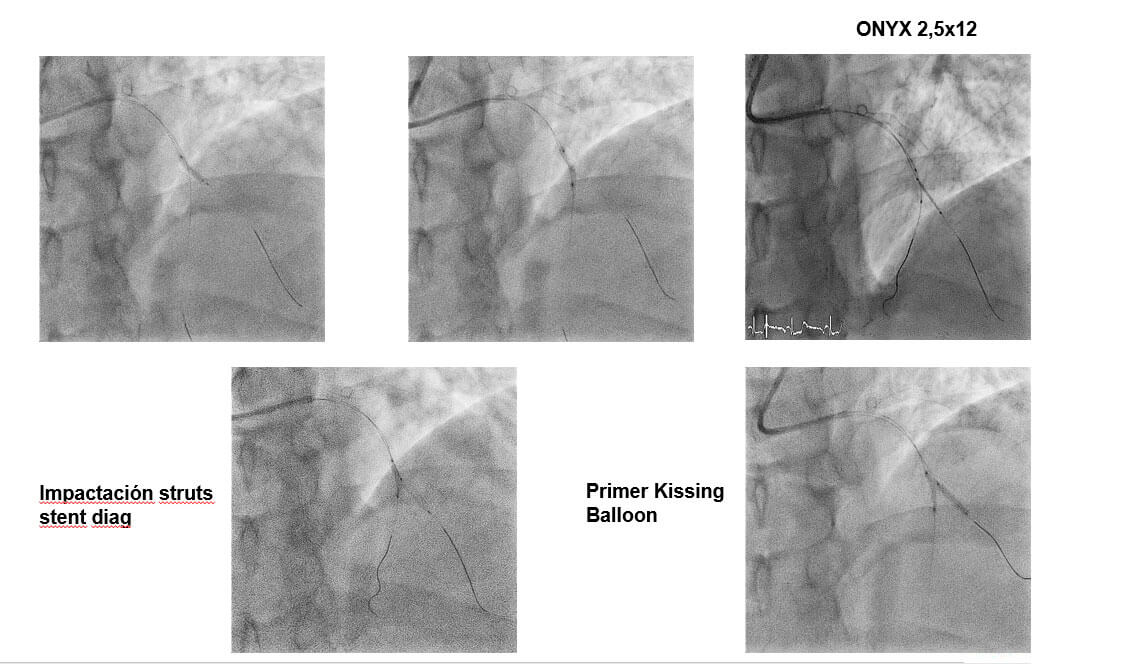
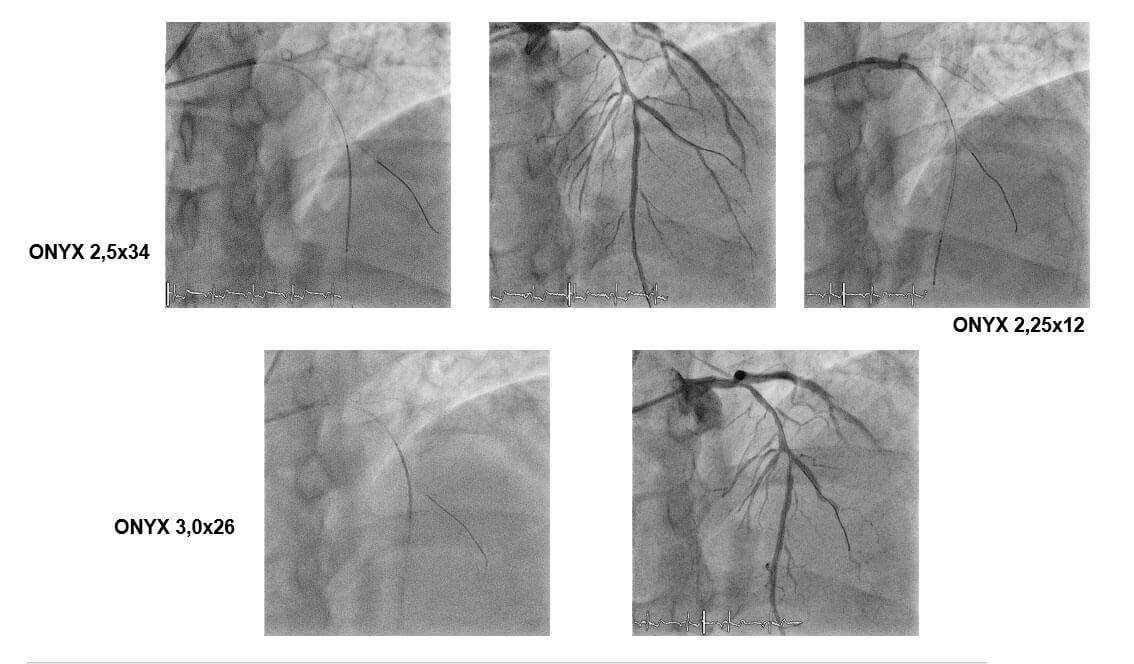
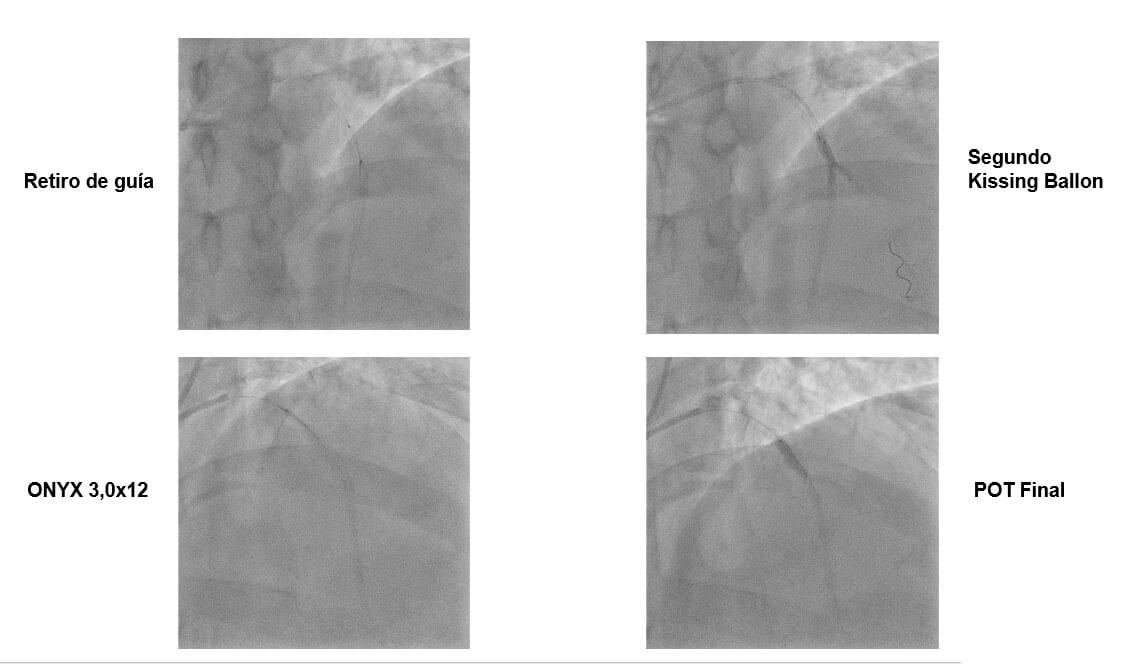
DK CRUSH: Step by Step
- Wire both MV and SB lesion with workhorse wire BMW 0,014.
- Predilate SB with balloon 2,0×12.
- Predilate MV with balloon 2,5×15 mm.
- Deploy stent to SB.
- Deploy SB ostium stent with balloon in LAD.
- Rewire SB stent ØKissing Balloon inflation.
- Deploy MV stents ØKissing Balloon inflation.
- Final POT.
Conclusions
- Using Double Crush Double Kissing to treat coronary bifurcation lesions is associated to reduced need of repeat revascularization compared against the Provisional Stent technique or other two-stent strategies, at present.
- The DKCRUSH strategy is more complex and requires a learning curve.
Expert Commentary: Dr. Carlos Uribe
This is quite a challenging case, since this is very a young fellow with elevated STEMI and associated multivessel disease.
- When should we revascularize RCA and LAD? Despite the ACC/AHA strong recommendation against treating multivessel disease in STEMI with PCI in one single action (from class III to IIB), the best practice in a stable patient is trying to do the left circumflex artery (LCX), and after 48 hours (same in hospital action) treat the remaining 2 arteries.
– Source: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000336
- What dual antiaggregation scheme would you indicate and for how long? Antiaggregation should be dual (DAPT) for at least 12 months, ideally with Ticagrelor or Prasugrel and ASA, leaving Clopidogrel for cases where the above mentioned drugs cannot be administered or are counter indicated (ESC/EACTS 2017 guidelines).
– Source: https://academic.oup.com/eurheartj/article/39/3/213/4095043
- ¿What PCI technique would you use to treat bifurcations? a) Provitional stent; b) CRUSH stent- Mini Crush stent; c) DK CRUSH stent; d) TAP stent; e) V o T stent
This is a remarkably interesting case to discuss. The left anterior descending has an exceptionally long lesion, with great D1 compromise, medina classification 1.1.1, which is traditionally left to a complex strategy with upfront 2-stent technique.
Although there is no universally accepted score to predict when a lesion should be treated with 1 or 2 stents, what we have learnt is that Medina classification alone is not enough (in this case 1.1.1); more importantly, we need to define the lesion as simple or complex, and so far, the closest and most valid score to do so was brought by the DEFINITION trial.
It appears that, of all the DEFINITION parameters, the most relevant and sensible is length, which looks at side branch (D1) lesion extension, whether more or less than 10 mm is compromised. This was emphasized in the most recent network meta-analysis by Gioia et al, in 2020:
Even though the EBC consensus recommends 5 mm length as criterion to define complexity and treat with upfront 2 stent technique, this criterion will most likely change, considering a SB (side branch) 10 mm lesion length criterion was also recently showed by Zimarino and cols registry analysis (representing the EBC) with 1252 patients, emphasizing the importance of this finding once again.
Therefore, in this case we see D1 shows 90% stenoses approx., but the lesion extends less than 10 mm along the side branch (D1), which is why I would recommend provisional stenting with one stent and, according to side branch (D1) evolution (considering sub-optimal over 75% of residual side branch compromise, or if left with residual dissection after branch POT-KB-POT), we could finalize with 1 additional stent (or bail-out) and consider a TAP or Culotte strategy according to experience and familiarity of operator.
In conclusion: initiate with 1 provisional stent and consider 1 additional stent if side branch evolution is sub optimal (2 stents in all).
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





