Intervention of chronic total occlusions (CTO) through angioplasty (PCI) can cause complications, even in highly experienced centers.

Plenty has been written on the probability of success for the treatment of CTOs using scores such as CL-SCORE, J-CTO, ORA, E-CTO, CASTLE-CTO, etc. (some of which are usually used when preparing these cases).
However, besides estimating success probability, we need tools to determine procedural risk, which is paramount for planning the intervention and informing the patient about its complexity.
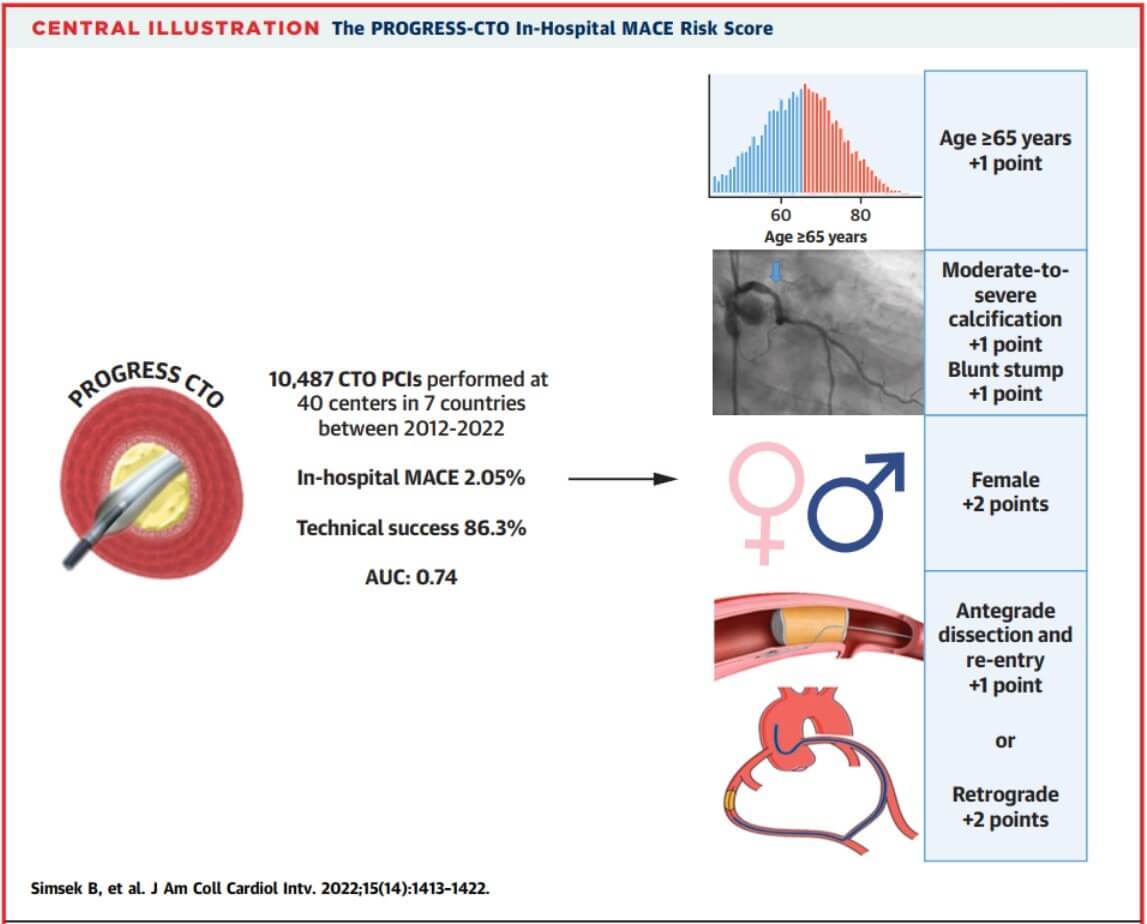
The aim of this study was to analyze the variables that carry the greatest risk and to update the initial score published 6 years ago. A study was conducted on data from a global prospective CTO registry, called PROGRESS-CTO, which included about 40 centers with high volume of CTO PCI.
Major adverse cardiac events (MACE) were defined as a composite of death, acute myocardial infarction (IAM), stroke, urgent revascularization, or pericardiocentesis. Procedural success was defined as technical success plus lack of in-hospital MACE. Demographic and technical variables were analyzed. Calcification was one of the parameters assessed: it was divided into mild (short segments), moderate (calcification ≤50% compared with baseline lesion diameter), or severe (≥50%).
Read also: Tricuspid Regurgitation: Edge-to-Edge Treatment with PASCAL.
Multivariate logistic regression was conducted, followed by ROC curves to determine the area under the curve (AUC) of the scores.
Out of 10487 cases of CTO PCI, MACE was observed during hospital stay in 2.05% of cases, with a mortality of 0.45%, AMI of 0.63%, and pericardiocentesis requirement of 1.08%. Patients who experienced MACE were generally older, mostly female, with moderate to severe calcification, major J-CTO score, and lower success with the antegrade chordae escalation strategy.
MACE, mortality, pericardiocentesis, and AMI risk scores were estimated. The score for predicting MACE included age (>65 years), sex (female, +2), moderate to severe calcification, crossing strategy (dissection and antegrade reentry [RD] +1 or retrograde +2), and occlusion stump (blunt or not), with an AUC of 0.74 (95% confidence interval [CI]: 0.70-0.78) and adequate internal validation.
Read also: Changes in Coronary Collateral Function Post CTO Intervention.
When assessing mortality, factors such as age, ventricular function, previous myocardial revascularization surgery, moderate to severe calcification, and the crossing technique (antegrade RD or retrograde stenting) were included, with an AUC of 0.80 (95% CI: 0.73-0.86).
The same was done for the risk of pericardiocentesis, with an AUC of 0.78 (95% CI: 0.72-0.83), while for AMI it resulted in an AUC of 0.72 (95% CI: 0.62-0.82).
Conclusions
This study made it possible to measure and internally validate 4 risk scores for CTO PCI, allowing for an update of the score previously presented 6 years ago (based on data from 1065 patients). It mainly has the limitation of observational data and the bias of a low number of complications due to the fact that these are high-experienced centers in this type of pathology, which partially limits its extrapolation.

Dr. Omar Tupayachi.
Member of the Editorial Board of SOLACI.org.
Original Title: Predicting Periprocedural Complications in Chronic Total Occlusion Percutaneous Coronary Intervention.
Font: J Am Coll Cardiol Intv. 2022 Jul, 15 (14) 1413–1422.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





