According to several registries, incomplete left atrial appendage (LAA) closure has been observed in up to 30% of cases after device implantation. The main cause of this complication is a mismatch between closure device and LAA ostium. The latter is elliptical in shape and varies in length, while the Watchman LAA closure device is round and comes in a limited number of sizes. This may result in incomplete sealing and peridevice leak (PDL), which in turn leads to blood stasis and thrombosis, and potential disruption of systemic circulation.

Large studies used to accept up to ≤5mm PDL to discontinue anticoagulation (warfarin) at day 45 and follow with dual antiaggregation (DAPT) for 6 months.
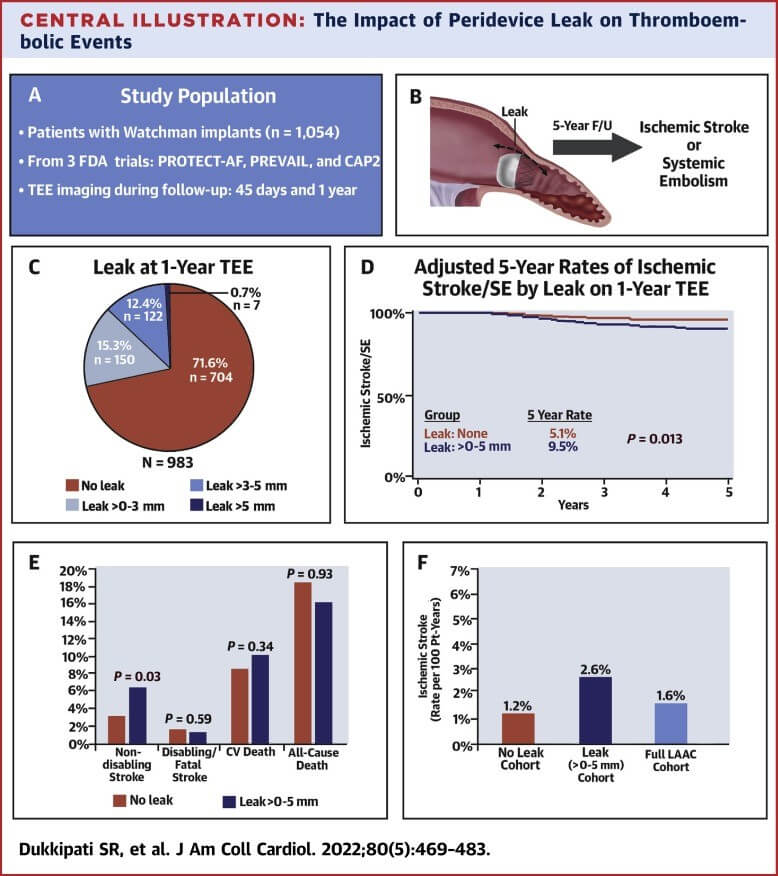
The aim of this study was to assess the behavior of PDL ≤5 patients at 5 years, vs. no PDL patients.
The study included patients from the randomized trials PROTECT-AF and PREVAIL and from the prospective CAP2 registry, all using Watchman 2.5 (5 sizes). Primary end points were ischemic stroke/ systemic embolism, cardiovascular death, and all-cause mortality.
They looked at 1054 patients, mean age 74, 65% men, CHA2DS2-VASC score = 4. There was no leak in 60.2% of cases and 38.3% presented PDL ≤5. At baseline, PDL patients presented more diabetes (34% vs 28%; p=0.033) and more history of ischemic stroke (17.6% vs 12.8%; P=0.033). Procedure related characteristics of PDL patients were longer LAA ostium (P=0.014), larger in diameter (P=0.002).
Read also: Longitudinal Deformation of a Stent with the POT Technique.
Patients with PDL were divided in subgroups with leak ≤3 at 45 days, which disappeared at followup in 47% of cases. While the subgroup with leak 3 to 5, it only disappeared in 24% of cases.
PDL ≤5 compared against absence of leak at 45 days was not significantly associated to risk of ischemic stroke or systemic embolization (9.2 vs 6.6; p=0.141), cardiovascular death (8.8 vs 10.3%;P=0.350) or all-cause mortality (18.5% vs 21.5%; P=0.350).
Transesophageal echocardiogram at one year, associated PDL with higher number of events, mainly ischemic and thromboembolic (HR: 1.92, IC 95% 1.14-3.25; P=0.0149) without higher cardiovascular mortality (10.1% vs 8.6%; p=0.382) or all-cause mortality (16.2% vs 18.3%; P=0.515). These variables showed the same results after adjusting.
Read also: Coronary Physiology Is Useful in Chronic Kidney Disease.
As regards stroke, PDL was associated to higher non-disabling stroke (HR 2.03, CI 95% 1.06-3.89; P=0.033), unlike fatal or disabling.
Conclusions
Small leaks (≤3) can reduce or even disappear (47%) after one year. However, their persistence after one year (≤5) was associated to nearly twice the risk of ischemic stroke or systemic thromboembolism at 5 years, mainly driven by non-fatal stroke (which matches surgical outcomes when closure is incomplete). However, this higher risk of cardiovascular events did not translate into increased mortality.

Dr. Omar Tupayachi.
Member of the Editorial Board of SOLACI.org.
Original Title: Impact of Peridevice Leak on 5-Year Outcomes After Left Atrial Appendage Closure.
Source: Dukkipati SR, Holmes DR Jr, Doshi SK, Kar S, Singh SM, Gibson D, et al. Impact of peridevice leak on 5-year outcomes after left atrial appendage closure. J Am Coll Cardiol. 2022;80(5):469-83. Disponible en: http://dx.doi.org/10.1016/j.jacc.2022.04.062.
Subscreva-se a nossa newsletter semanal
Receba resumos com os últimos artigos científicos





