
New clinical case from SOLACI PERIPHERAL!
This time, we present a case featuring an abdominal aortic aneurysm with hostile neck. With this, we wrap up an intense year during which we published 5 clinical cases to deepen and stimulate the exchange between Latin American interventionist colleagues.
Tell us what you think about this case using the comments section in this post, and answer the questions featured in the last part of this article.
Abdominal Aortic Aneurysm with Hostile Neck
Authors: Dr. Maximiliano Rossi, Dr. Anibal Damonte, Dr. Fernando Kozak, and Dr. Leandro Lasave.
E-mail: maxicrossi@hotmail.com Twitter: @MaxicRossi.
Site: Rosario Cardiovascular Institute, Santa Fe, Argentina.
60-year-old patient.
Cardiovascular risk factors:
- High blood pressure
- Smoking
- Sedentary lifestyle
- Overweight
- Dyslipidemia
Cardiovascular disease history:
- Ischemic heart disease with moderate impairment of the ejection fraction.
- 2015: Acute infero-lateral-dorsal myocardial infarction reperfused through primary angioplasty to the right coronary artery; incomplete revascularization.
Assessments conducted:
- Stress/rest cardiac SPECT (October 19th, 2016): Inferior fibrosis (fibrosis level: 19%). Mild residual ischemia. Ejection fraction 39%.
- Doppler echochardiogram (February 13th, 2017): Ejection fraction 40%. Inferior akinesia in all segments. Laterobasal, lateromedial hypokinesis. No valve disease.
Other conditions:
- Chronic obstructive pulmonary disease.
- Spirometry (November 11th, 2016): Moderate to severe restriction.
For non-specific abdominal and lumbar pain spanning for months, an abdominal ultrasound is conducted; it shows a 54-mm diameter abdominal aortic aneurysm.
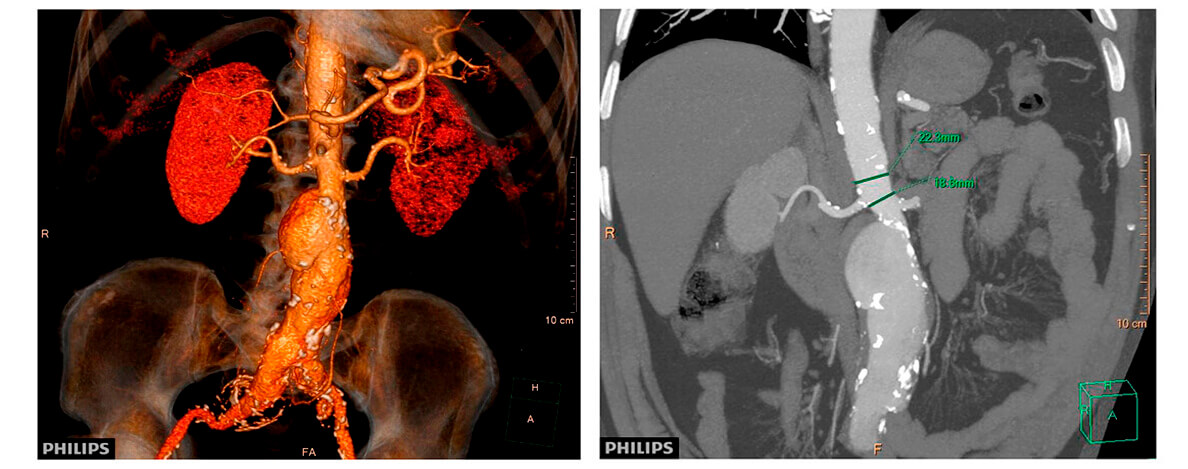
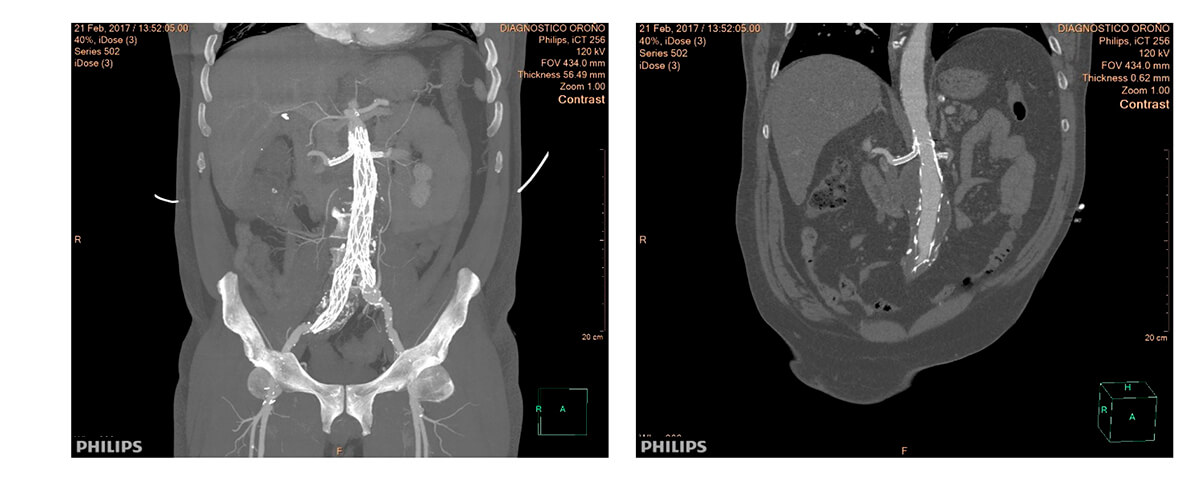
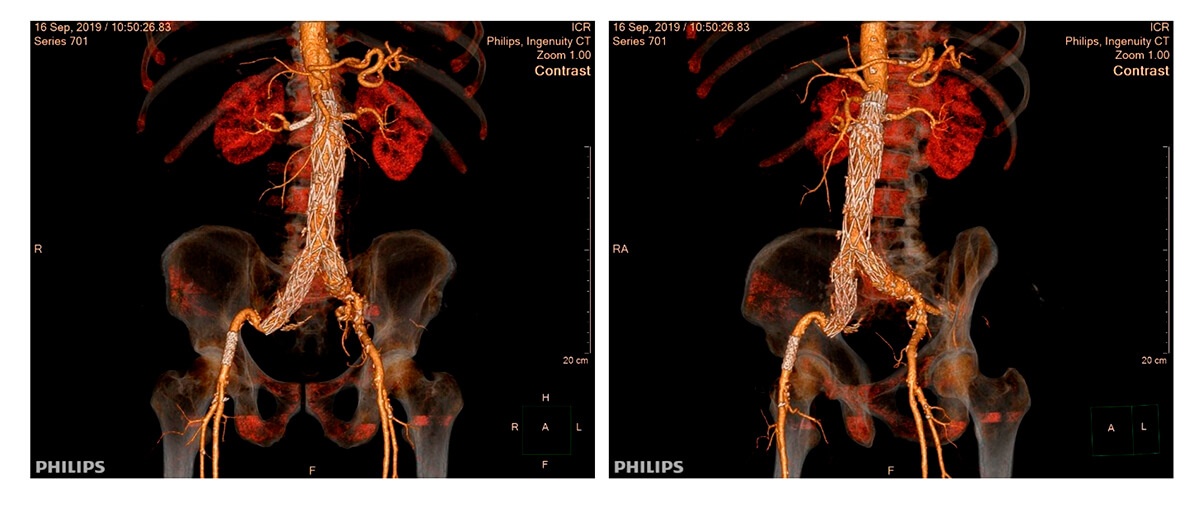
A multi-slice computed tomography (CT) of the abdominal aorta is requested.
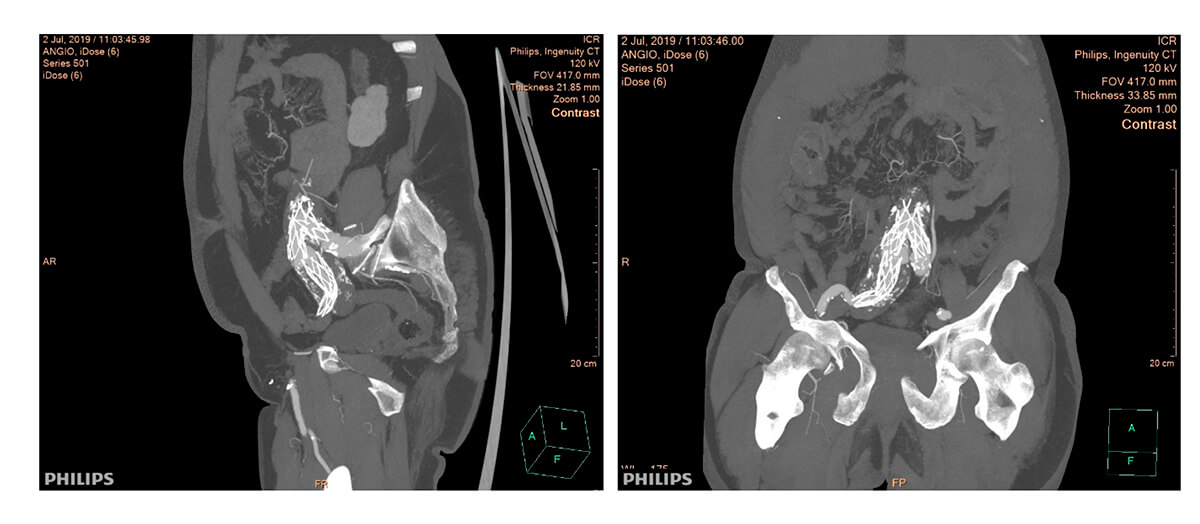
Multi-slice TC imaging
After a joint evaluation with the cardiovascular surgery and the hemodynamics services, the patient is considered of high surgical risk. A decision is made to conduct an endovascular exclusion.
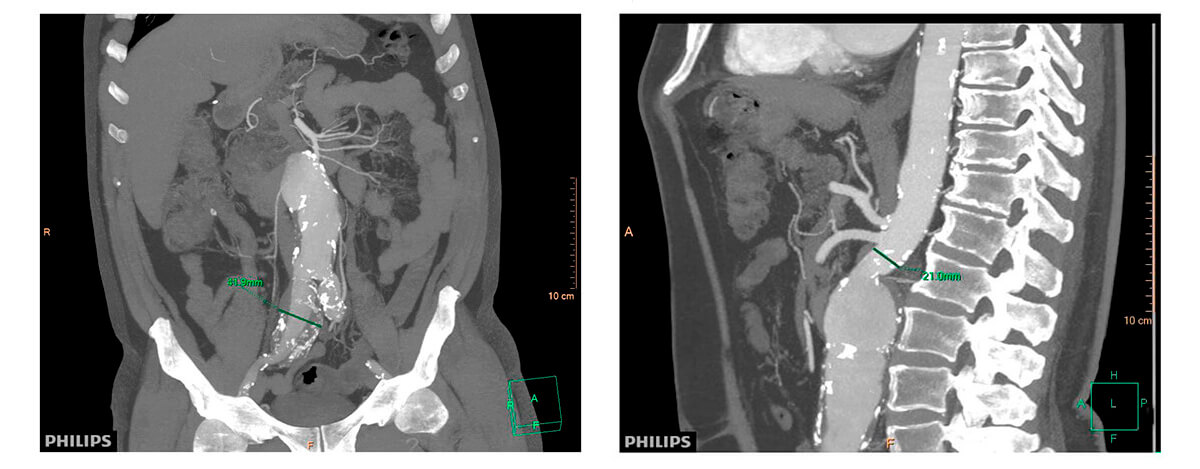
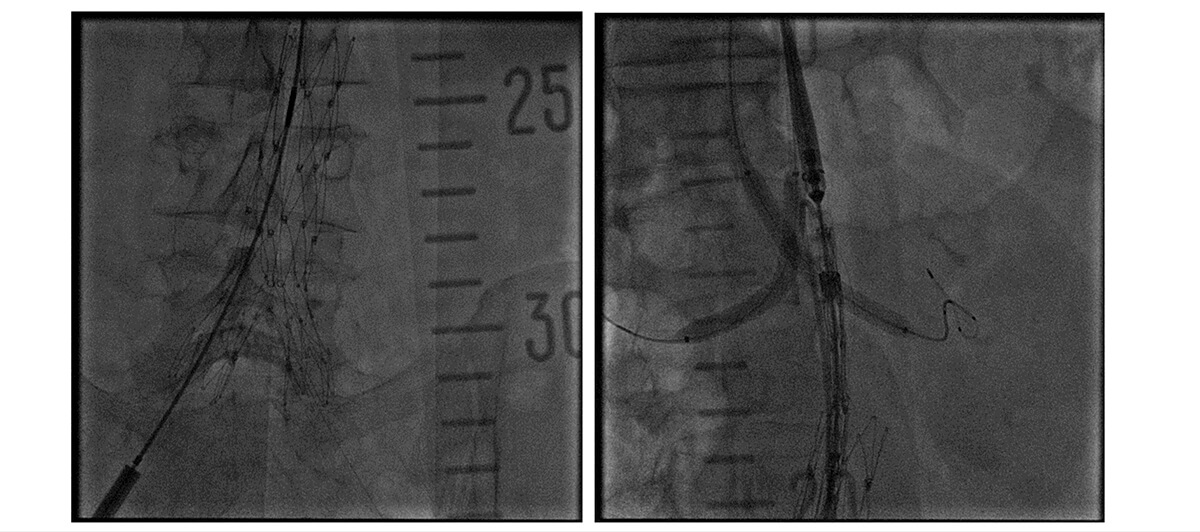
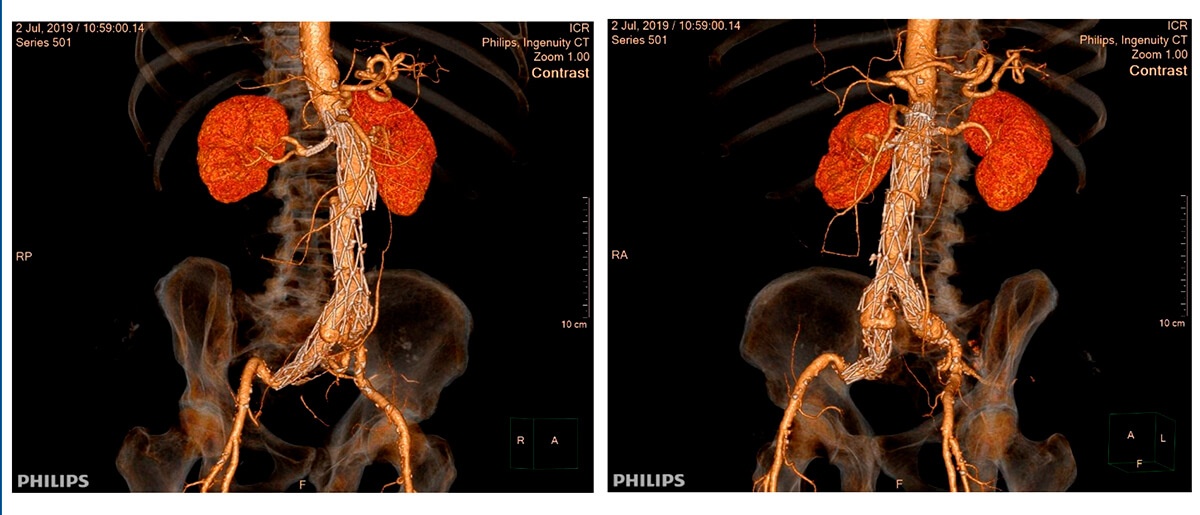
Procedure
- Endovascular exclusion of the aorto-iliac aneurysm with chimney construction to both renal arteries.
- Surgical vascular access in the right femoral artery and access by puncture in the left femoral artery.
- Puncture access in both brachial arteries for renal stent implantation.
- Prosthesis provided by AFX Endologix. The device used had a 22-mm proximal diameter and a 20-mm branch diameter, and it was 120 mm long. The Vela Cuff had a 25-mm diameter × 75-mm length, and its right iliac extension had a 20-mm proximal diameter, a 13-mm distal diameter, and its length was 90 mm.
- The telescope length achieved between body and proximal cuff was 25 mm, with a 22-mm right iliac extension.
- Advanta V12 stents were used. Two 6.0-59 mm stents were used for each renal artery.
- Simultaneous post-dilation of proximal neck and chimneys.
Procedure imaging
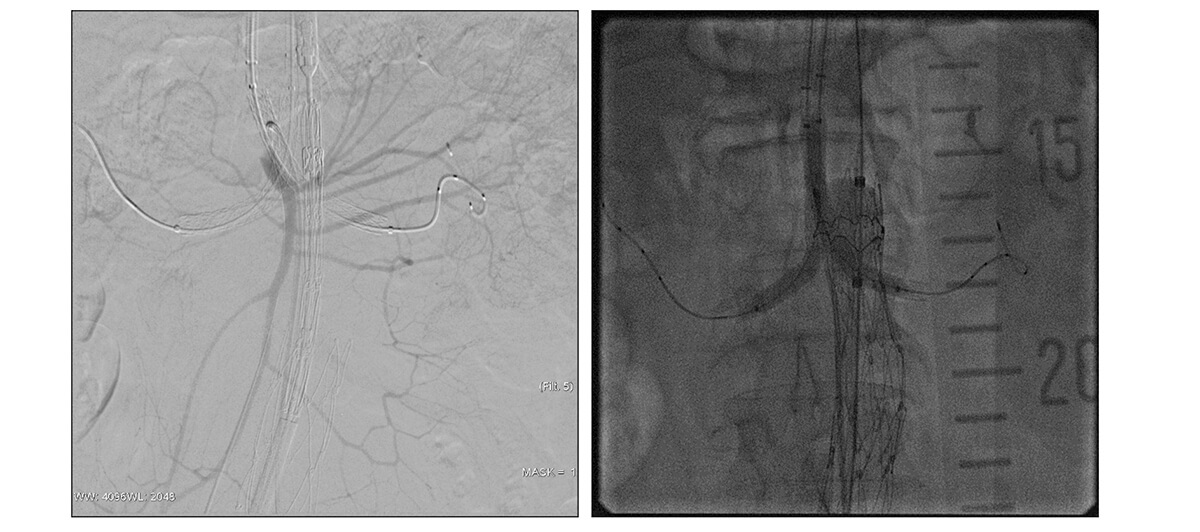
Follow-up at 3 months and 1 year: no leak and patent chimneys.
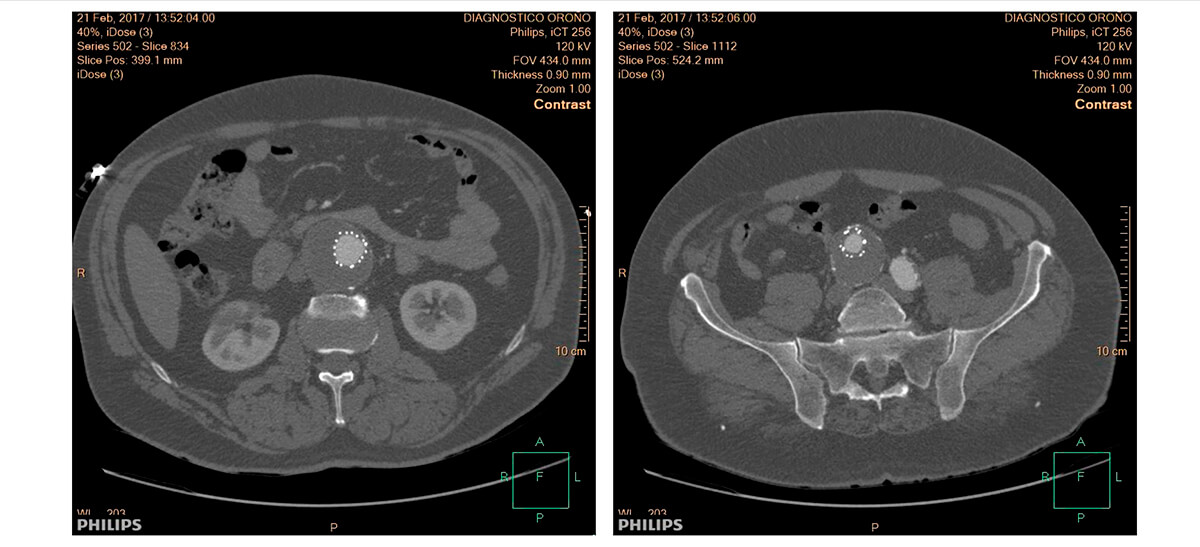
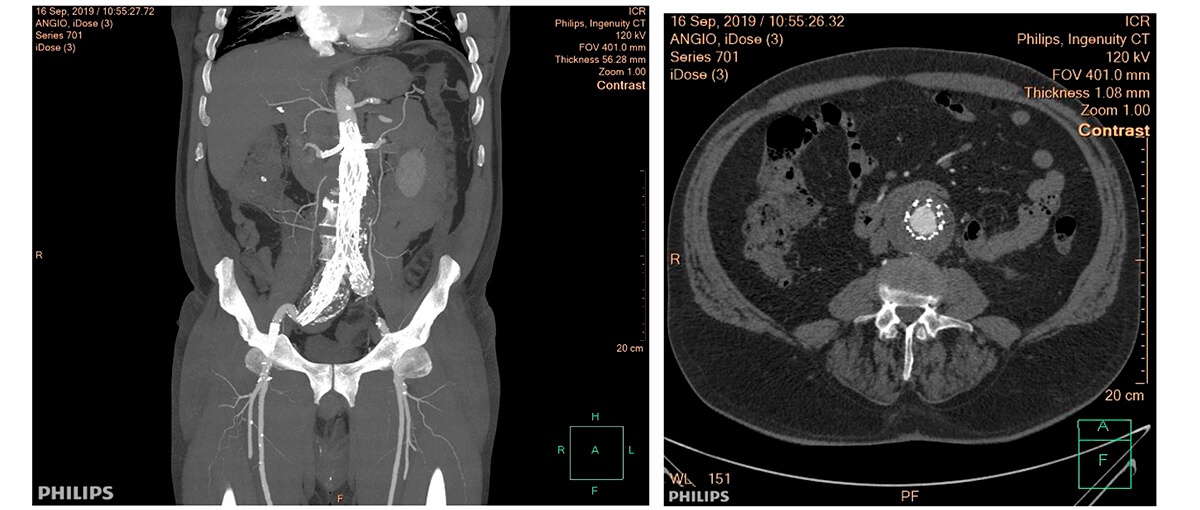
Multi-slice TC after 3 months of follow-up
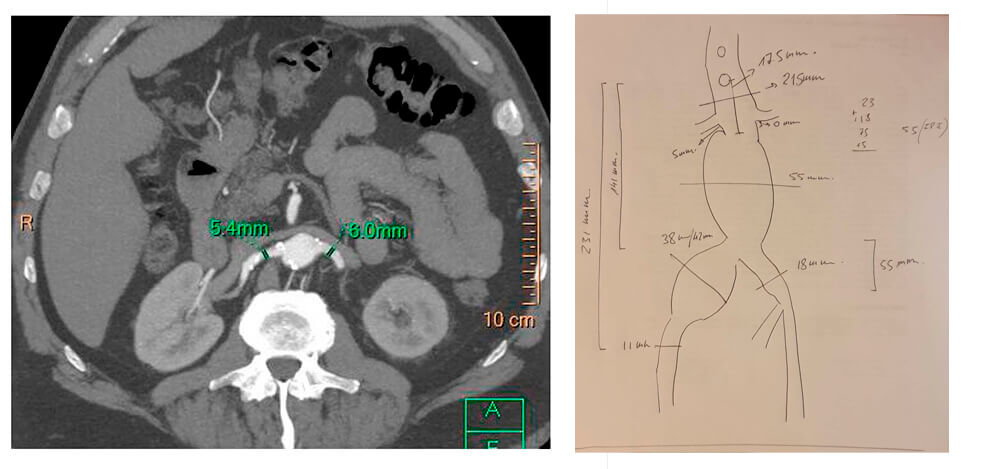
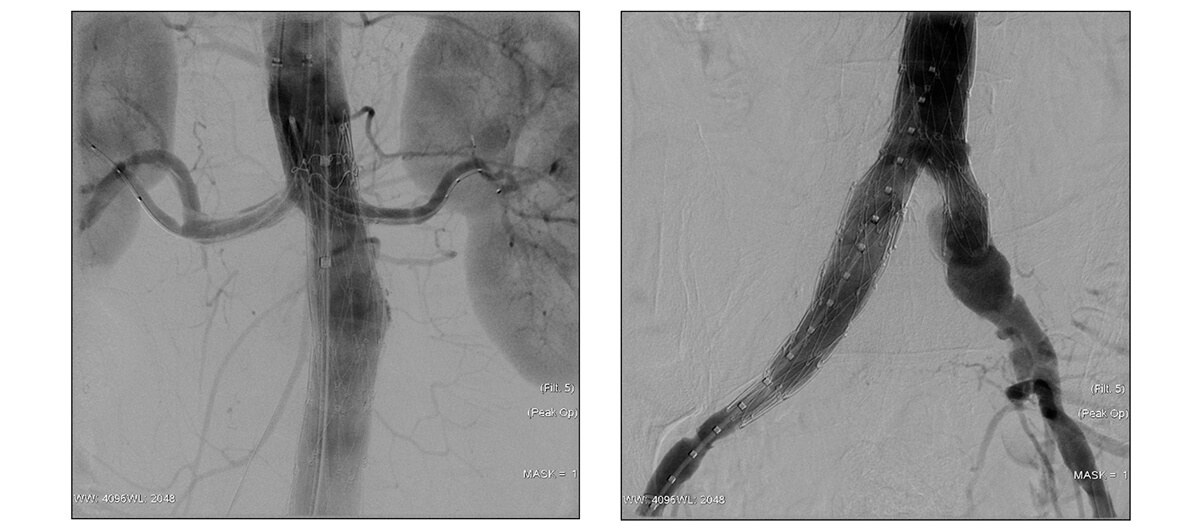
Two-year follow-up.
Multi-slice TC after 2 years of follow-up
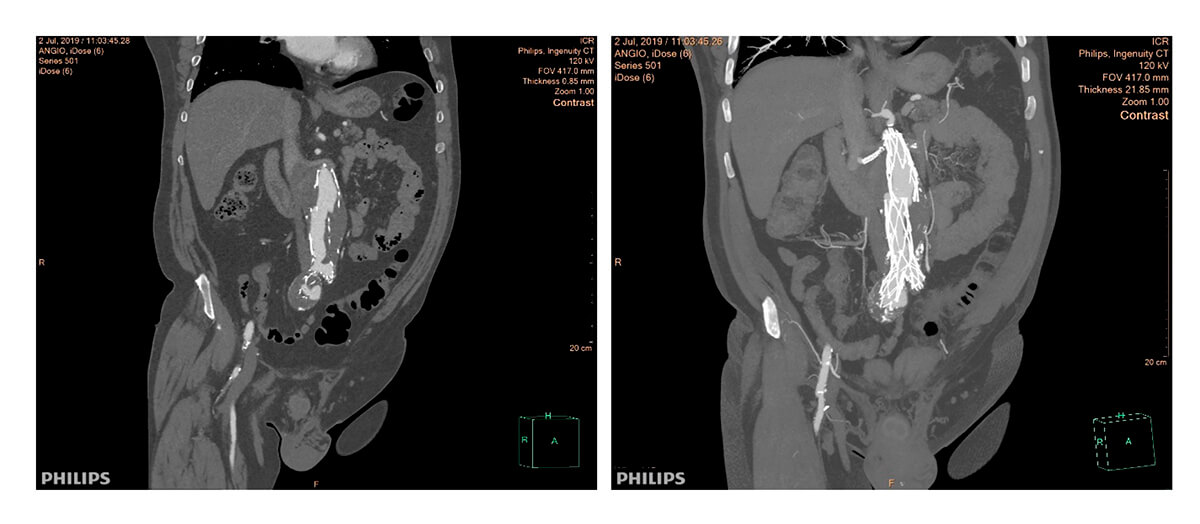
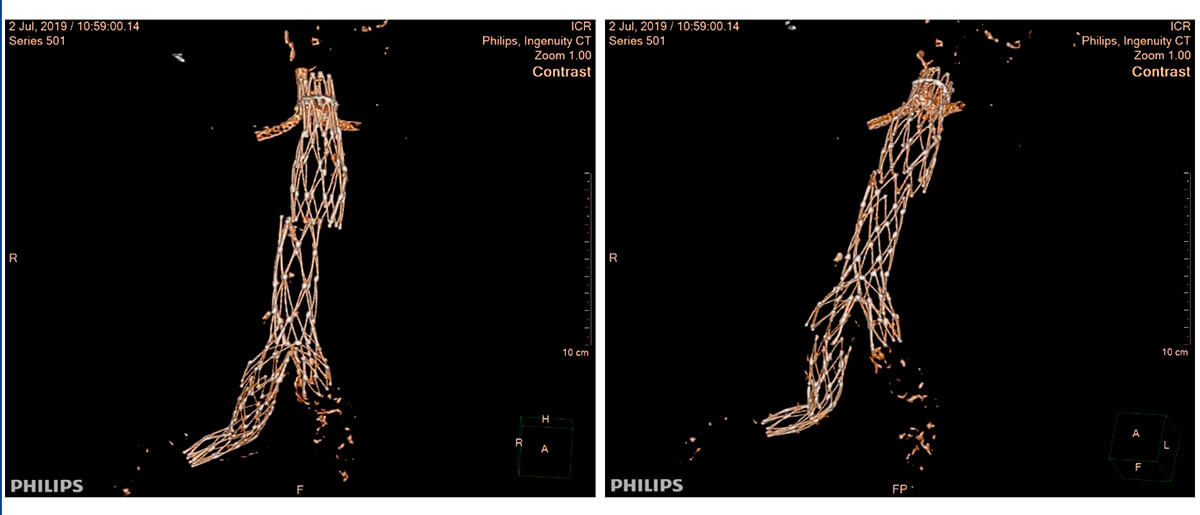
Type III leak due to body decoupling with proximal cuff and right iliac branch of the body decoupling with iliac extension. Both disconnections with little solution for continuity, misaligned and without overlapping between the prostheses.
Procedure:
- Endovascular repair of type III leak.
- Right transradial access for angiographic control.
- Right percutaneous access (same surgical access previously used). Two PROGLIDE percutaneous sutures applied.
- Aortic cuff: 28 mm diameter × 95 mm long. Conical iliac extension: 20 mm proximal, 13 mm distal, and 90 mm long.
- Due to failure of the right percutaneous femoral access closure and perforation of the common femoral artery, a BeGraft 9-37 mm covered stent is implanted by contralateral and cross-over access.
Procedure imaging
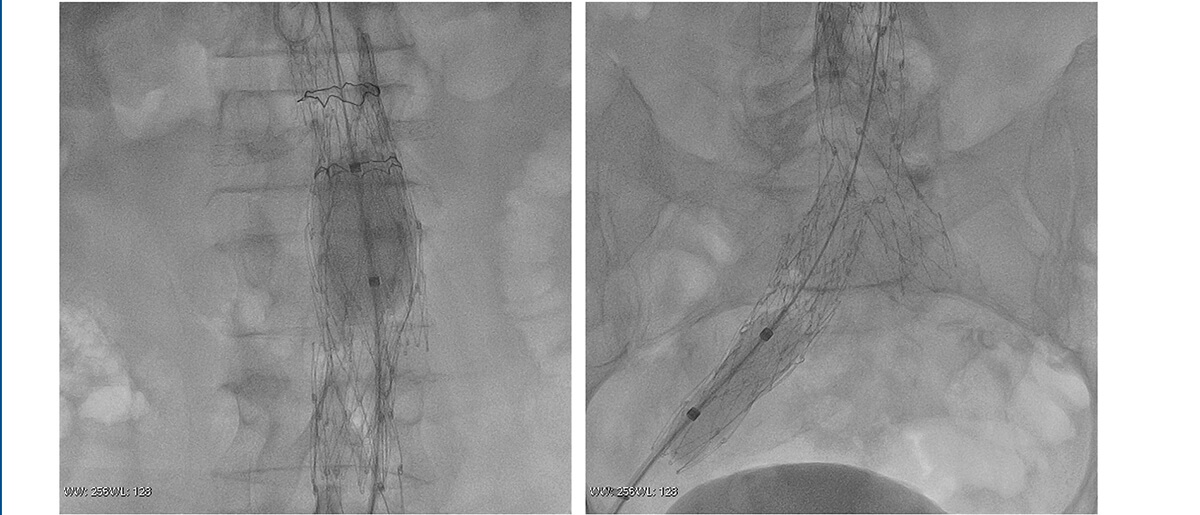

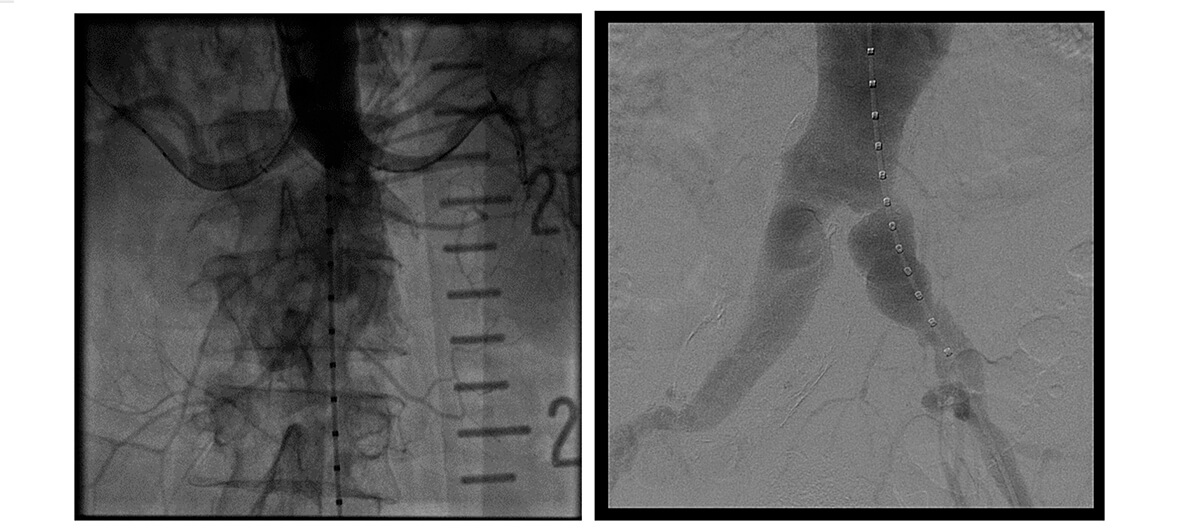
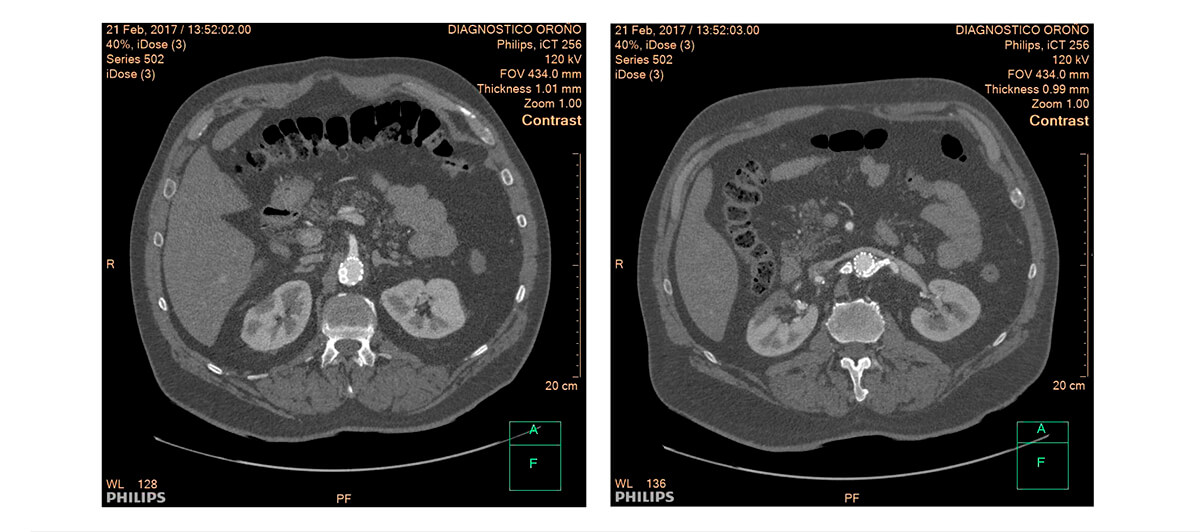
Follow-up at 3 months. No leak.
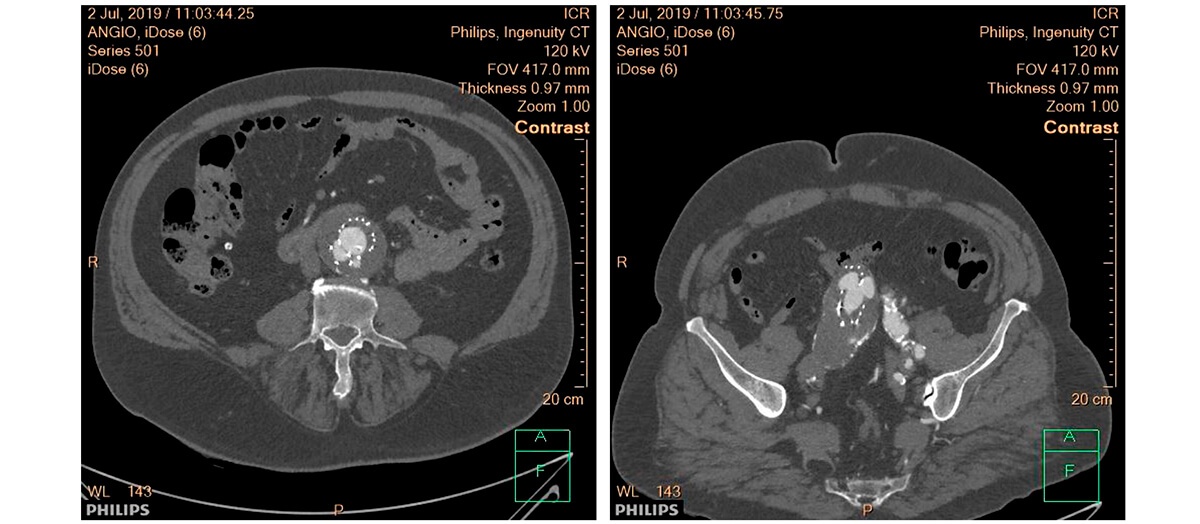
Multi-slice TC after 3 months of follow-up
Questions:
- Do you believe that the most appropriate initial indication is open surgery, despite the increased surgical risk?
- Would you have chosen a different endovascular option to treat this aneurysm?
- Do you think that a stricter post-exclusion monitoring of AAA is necessary with certain prostheses or techniques?
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





