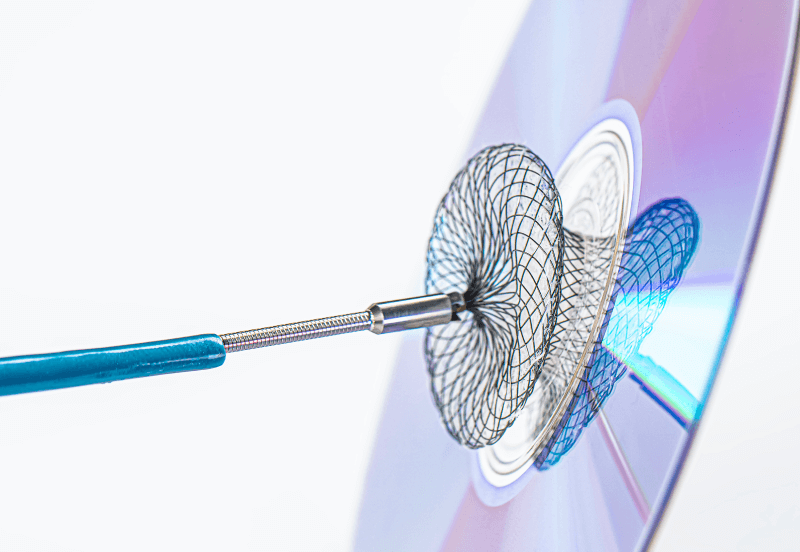
Courtesy of Dr. Juan Manuel Pérez.
Percutaneous left atrial appendage occlusion (LAAO) is an alternative to oral anticoagulation (OAC), albeit one that still poses some questions remain regarding its indications, the need for preprocedural imaging, the postprocedural antithrombotic regimen, and its potential complications.
The 2025 SCAI/HRS technical review structures evidence around eight key questions aimed at guiding clinical practice:
LAAO vs no anticoagulation?
A single study compared LAAO with no OAC in patients with end-stage renal disease on hemodialysis. LAAO was associated with lower mortality rates (hazard ratio [HR] 0.52), fewer thromboembolic stroke events (HR 0.16), and less major bleeding (HR 0.51).
LAAO vs OAC?
The PROTECT-AF (n=707), PREVAIL (n=407), and PRAGUE-17 (n=402) trials, with follow-ups of 40 to 60 months, showed lower all-cause mortality (HR 0.76), cardiovascular mortality (HR 0.64), and non-periprocedural bleeding (HR 0.52) rates with LAAO compared with OAC. However, there was a higher risk of ischemic stroke (HR 1.52), with no differences in total stroke or major bleeding.
Read also: Clinical Impact of Peridevice Leak Following Left Atrial Appendage Closure.
Is preprocedural imaging (transesophageal echocardiography or computed tomography) necessary?
Two observational studies indicated that skipping preprocedural imaging reduced procedural success rates (risk ratio [RR] 0.87) and increased contrast and radiation use, underscoring the importance of planning with transesophageal echocardiography (TEE) or computed tomography (CT).
Intracardiac echocardiography vs transesophageal echocardiography during implantation?
Six non-randomized studies, including the NCDR LAAO Registry (>34,000 patients) and European multicenter registries, reported similar outcomes for success, stroke, bleeding, and leak. Mortality was higher with intracardiac echocardiography (ICE), a fact most likely related to the learning curve.
What is the best post-implant therapy: OAC or antiplatelet therapy?
An analysis of the NCDR LAAO Registry (>34,000 patients) showed comparable outcomes between OAC and dual antiplatelet therapy (DAPT) regarding stroke, bleeding, and thrombosis, although DAPT might be associated with higher mortality rates (RR 1.31). Evidence on single antiplatelet therapy (SAPT) is still uncertain and of very low quality.
Read also: Evolution of Renal Denervation at 24 Months.
Should there be postprocedural follow-up with TEE or CT?
Registries reported device-related thrombosis in 1.6–4.1% of cases and significant leak in <3%. However, no studies have compared patients with and without follow-up imaging, so it remains unclear whether systematic TEE or CT improves outcomes. In the initial trials, follow-ups were performed at 45 days and one year, but there is currently no consensus on their necessity or frequency.
Should OAC be indicated in patients with peridevice leak (PDL)?
A subanalysis of PROTECT-AF showed that maintaining OAC did not reduce stroke events (HR 0.85), even in cases of leak >5 mm.
Indefinite OAC in device-related thrombosis (DRT)?
Five retrospective studies (n=400; follow-up 1–21 months) suggest that OAC may favor thrombosis resolution (RR 1.13), although at the cost of increased bleeding (RR 1.73), without clear evidence of stroke reduction.
Conclusion
The review confirms that LAAO is an effective alternative to OAC, with benefits in mortality and bleeding reduction demonstrated in randomized clinical trials. However, for most other issues—use of imaging before and after the procedure, choice between ICE or TEE, type and duration of antithrombotic therapy, and management of leak or thrombosis—the evidence comes mainly from observational studies and registries, with low or very low certainty. This highlights the urgent need for new randomized trials to standardize protocols and maximize the clinical benefit of LAAO.
Original Title: SCAI/HRS Technical Review on Transcatheter Left Atrial Appendage Occlusion.
Reference: Edmond M. Cronin et al. Heart Rhythm, 2025; -:1–11. https://doi.org/10.1016/j.hrthm.2025.05.049.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





