According to this recent document by the American Heart Association (AHA), troponin should be monitored for at least 3 days after surgery.
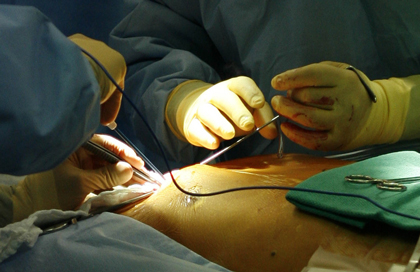
With about 20% of patients (most of them, asymptomatic) showing elevated troponin after a non-cardiac surgery, this new AHA document recommends monitoring, for at least two days, patients with moderate to severe ischemia.
Myocardial injury after non-cardiac surgery was first associated with increased mortality in 2014. At the time, researchers interpreted that these events could be triggered by an increased burden of risk factors, including patients over 75 years of age with sleep apnea, anemia, cardiac failure, diabetes, and hypertension.
The moral of this work would be that myocardial injury after non-cardiac surgery is frequent, silent, and fatal—so it should be taken into account.
Current evidence shows that patients who develop injury have four times higher 30-day mortality, and about 90% of this population has no identifiable symptoms.
Given that most subjects develop symptoms within 24 hours, the document suggests dosing troponins for 48 to 72 hours in patients at moderately high risk.
Read also: Hypertensive Patients: Maximizing Doses or Adding New Drugs.
The idea of performing ischemia-evoking tests prior to non-cardiac surgery left us without much to do if a patient with normal results developed an injury. Now we can comprehend the elevation and re-stratify patients, reducing their future risk.
Post-surgical injury should end in a direct referral to a cardiologist to evaluate the indication for aspirin and lifestyle changes. Patient could interpret this as secondary prevention.
CIR-0000000000001024Original Title: Diagnosis and management of patients with myocardial injury after noncardiac surgery: a scientific statement from the American Heart Association.
Reference: Kurt Ruetzler et al. Circulation. 2021 Oct 4;CIR0000000000001024. Online ahead of print. doi: 10.1161/CIR.0000000000001024.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





