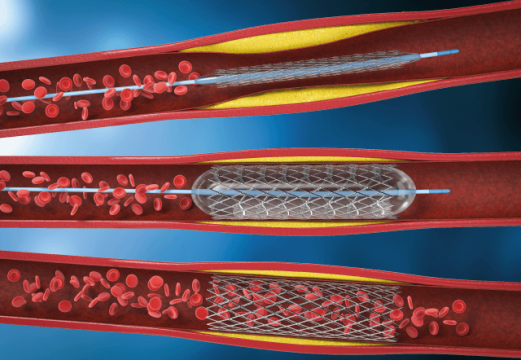
The prevalence of coronary lesions with bifurcation involvement is about 20% in patients undergoing coronary angiography (CTA). While provisional stenting is overall the most accepted technique, the 2018 myocardial revascularization guidelines recommend the 2-stent technique for complex bifurcation lesions, defined as side branch with lesion >5mm, distal reference diameter of the side branch ≥2.75, or difficulty in accessing the side branch prior stent implantation in the main vessel.
Prospective, multicenter, randomized study DEFINITION II reported a significant improvement in clinical outcomes after one year using the 2-stent technique in patients with complex coronary bifurcation lesions. However, there is no long-term information on the benefit of these techniques.
The purpose of this study was to evaluate the 3-year follow-up clinical outcomes after the 2-stent technique vs. provisional stenting.
The primary endpoint (PEP) was treated lesion failure (TLF), which included cardiovascular death, treated-vessel-related acute myocardial infarction (AMI), and clinically driven repeat vascularization of the treated vessel (TVF). The safety endpoint was stent thrombosis.
The study enrolled 635 patients, 328 in the 2-stent arm and 325 in the provisional stenting (PS) arm. Mean patient age was 63 years old, and most subjects were male. Of all patients, 34% had diabetes, and the most frequent clinical presentation was unstable angina.
In the PS arm, 22% of patients needed a side branch stent due to suboptimal outcomes. Furthermore, side branch pre-treatment increased the need for additional stent use in the PS arm (32% vs. 14%, p < 0,001). There were no differences between arms in POT and kissing balloon use. The intravascular ultrasound (IVUS) use rate was 27%.
Read also: Same Day Discharge in NSTE-ACS: Is It Possible?
The 3-year PEP was 16% in the PS arm and 10% in the 2-stent arm (hazard ratio [HR]: 0.63; 95% confidence interval [CI]: 0.41-0.97; p = 0.035). There was a predominance of increased AMI (8.0% vs. 3.7%; HR: 0.63; 95% CI: 0.41-0.97; p =0.035) and treated vessel revascularization (HR: 0.50; 95% CI: 0.26-0.96; p = 0.038) in the PS arm. There was no difference in the safety endpoint between the two arms.
Among patients in the PS arm, patients requiring 2 stents had higher TLF rates, which was attributed to the high rate of repeat revascularization. Finally, patients who experienced intraprocedural complications had a higher rate of TLF at 1 year compared with patients with no complications.
Conclusion
The risk of future events remains present for patients with complex coronary bifurcation lesions with no events 1 year after the procedure.
Dr. Andrés Rodríguez.
Member of the Editorial Board of SOLACI.org.
Original Title: 3-Year Outcomes After 2-Stent With Provisional Stenting for Complex Bifurcation Lesions Defined by DEFINITION Criteria.
Reference: Jing Kan, MBBS et alJ Am Coll Cardiol Intv 2022;15:1310–1320.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





