The clinical importance of severe tricuspid regurgitation (TR) has been underestimated for many years now. However, studies and registries have shown that, when left untreated, this pathology significantly increases morbidity and mortality. Patients in need of treatment are often older individuals with higher surgical risk due to the prevalence of this condition.
Contemporary data has shown that surgical treatment carries high perioperative mortality rates (6%-12%), which limit its use in the aforementioned population.
Fortunately, the possibility of a non-surgical and less invasive alternative has shown promising initial results. In the TRILUMINATE study, tricuspid transcatheter edge-to-edge repair (T-TEER) has been demonstrated to be safe and effective in reducing the severity of TR and improving the quality of life in the selected cohort.
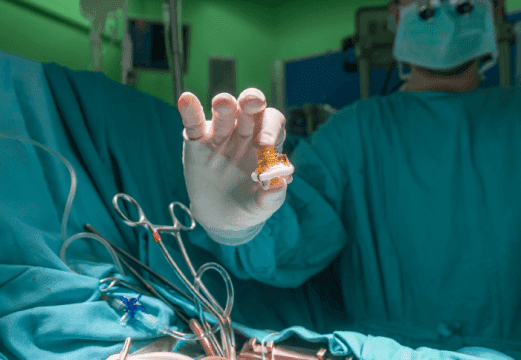
On the other hand, the bRIGHT study (an observational study) included real-world patients treated with the TriClip (Abbott) device. This is the first prospective and multicenter registry assessing safety and performance in an unselected contemporary cohort. The primary endpoint was acute procedural success (APS), defined as successful implantation with at least one-grade reduction in TR severity. Consecutive patients from 26 sites in Europe with severe symptomatic TR despite optimal medical treatment were eligible to undergo T-TEER.
The study included a total of 511 patients (56% female) with an average age of 79±7 years. In most cases, TR had a functional mechanism (90%), and 80% of patients were in New York Heart Association (NYHA) class III or IV, with an average Kansas City Cardiomyopathy Questionnaire (KCCQ) score of 43.1±23.7. About 27% of patients had undergone a prior mitral intervention, and 40% had been hospitalized for heart failure in the year prior to the procedure.
Echocardiographic findings revealed right ventricular dilatation (average diastolic diameter of 4.63±0.92 cm) with increased annular diameter (4.54±0.76 cm) in approximately 47% of cases and a gap of 7 mm or more.
Implantation was successful in 99% of cases, with APS achieved in 451 (91%) of the 496 patients. On average, 1.9±0.7 clips were used during the procedure, which had a mean duration of 76±39 minutes. At discharge, 80% of patients treated with the device had a moderate or less TR severity (compared with 2% at baseline). Multivariable logistic regression identified right atrial volume (RAV) and lower baseline TR severity as independent predictors of moderate or less reduction in TR (odds ratio [OR]: 0.726; 95% confidence interval [CI]: 0.572-0.921; P = 0.0085; OR: 0.371; 95% CI: 0.223-0.617; P = 0.0001).
From a clinical perspective, procedural success was observed through an improvement in patient functional classification, with an increase from 20% to 79% in NYHA class I to II (P < 0.0001), and an average increase of 19±23 points in the KCCQ quality of life score.
Read also: Are There Sex Differences in pLVAD-Assisted High Risk PCI?
At 30 days, all-cause mortality was 1%, and the reported rate of major adverse events (MAE) was 2.5%. Other safety events included a low rate of tricuspid reintervention (0.2%) and of reoperation (0.4%), a 7.2%-rate of major bleeding (BARC), and a 3.8%-rate of device fixation failure (single valve) (n = 17).
Conclusions
The preliminary results of bRIGHT showed a low rate of MAE and 30-day mortality, with a demonstrable clinical effectiveness profile at 30 days, resulting in an improvement in quality of life.

Dr. Omar Tupayachi.
Member of the Editorial Board of SOLACI.org.
Original Title: Short-Term Outcomes of Tricuspid Edge-to-Edge Repair in Clinical Practice.
Reference: Lurz, Philipp et al. “Short-Term Outcomes of Tricuspid Edge-to-Edge Repair in Clinical Practice.” Journal of the American College of Cardiology vol. 82,4 (2023): 281-291. doi:10.1016/j.jacc.2023.05.008.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





