Coronary bifurcation lesions have been a subject to debate, with different approaches by various medical teams. These lesions often carry a higher risk of ischemic events compared with lesions at non-bifurcated sites. The main strategy, supported by medical society recommendations and clinical guidelines, involves using provisional stenting with one stent to minimize the number of devices used.
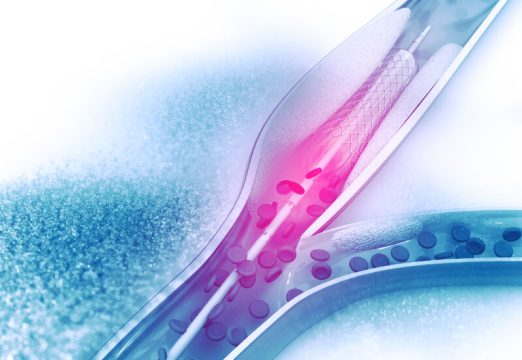
Recent studies focused on treating bifurcation lesions have shed light on Medina 0.0.1-type lesions, characterized by ostial involvement of the side branch, and have shown that these have the worst prognosis compared with other bifurcation lesions.
While these account for less than 5% of cases, most previous studies on this topic included a small number of patients with these characteristics. Therefore, the purpose of this study was to compare the use of one or two stents in Medina 0.0.1-type lesions using patient data collected in the extended BIFURCAT registry, which combines data from the RAIN, COBIS II, and III registries.
Of all the patients registered in RAIN (2889 patients), COBIS II (2897 patients), and COBIS III (2648 patients), only 4.1% had Medina 0.0.1-type lesions. Among these patients, 60.6% received a single stent, while the remaining 39.4% underwent 2-stent implantation. The primary endpoint (PEP) assessed was the presence of major adverse cardiovascular events (MACE), which included a combination of all-cause mortality, myocardial infarction, target vessel revascularization, and stent thrombosis.
Read also: Use of Drug-Coated Balloons in De Novo Lesions in Large Coronary Vessels.
Overall, patients undergoing the two-stent strategy had a higher incidence of involvement of the left main coronary artery (49.3% vs. 24.9% with one stent; P<0.001) and calcified lesions (24.3% vs. 11.5% with one stent). In terms of timing, there was a gradual increase in the preference for the provisional strategy over time, with 76.1% of the procedures including strut opening, while the rest were limited to crossover from the main vessel to the side branch. In the two-stent strategy, the most common technique was “crush” (56.6%), followed by “T-stenting” and “TAP” (24.3%). Approximately one-third of patients had involvement of the circumflex side branch, and there was greater use of intravascular imaging when two stents were used (52.9% vs. 45.9%).
The average patient follow-up was 800 days. In the entire registry cohort, Medina 0.0.1-type lesions had the highest incidence of MACE (13.9%). The choice of using one or two stents did not have a significant impact on the MACE rate (14.3% vs. 13.9%; HR 1.034, 95% CI: 0.541-1.977; P=0.92), and these results remained consistent even after sensitivity analysis.
Furthermore, patients were stratified into three groups (procedure with one stent and only crossover, procedure with one stent and strut opening, and two-stent strategy), and no significant differences were found in terms of the PEP (13.5% vs. 14.4% vs. 13.9%; P=0.86).
Conclusions
In summary, bifurcation angioplasty is considered a complex procedure that entails a higher risk of events compared with other lesions. According to the results of this registry, Medina 0.0.1-type lesions, with ostial involvement of the side branch, are associated with a higher incidence of MACE. Regarding treatment strategy, no significant differences were observed in terms of MACE between the use of one or two stents. It is important to note that due to the observational nature of the study and the lack of a medical treatment group, definitive conclusions cannot be drawn, but the impact of side branch lesions on clinical outcomes becomes clear.

Dr. Omar Tupayachi.
Member of the Editorial Board of SOLACI.org.
Original Title: Comparison of Outcomes Between 1- and 2-Stent Techniques for Medina Classification 0.0.1 Coronary Bifurcation Lesions.
Reference: Choi, Ki Hong et al. “Comparison of Outcomes Between 1- and 2-Stent Techniques for Medina Classification 0.0.1 Coronary Bifurcation Lesions.” JACC. Cardiovascular interventions vol. 16,17 (2023): 2083-2093. doi:10.1016/j.jcin.2023.06.013.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





