
New SOLACI PERIPHERAL clinical case to keep learning among peers!
Dr. Carlos Eduardo Díniz Couto shares a “Nutcracker” case from Belo Horizonte, Brazil. This is the 7th clinical case presented by SOLACI Peripheral on the SOLACI website.
This space is intended to further promote and share experiences and opinions in order to continue improving our knowledge of interventional cardiology.
Join the discussion through the comments in this article!
Percutaneous Treatment for Nutcracker Syndrome
Author: Carlos Eduardo Diniz Couto (Brasil)
Contact: Carlos.Eduardo@hsemper.com.br.
Institution: Hospital SEMPER. Belo Horizonte – Minas Gerais, Brasil
Vea los otros casos clínicos de SOLACI Peripheral publicados en nuestra web.
Medical record
- Female patient, 38 years old, no comorbidities.
- Dyspareunia, dysuria, pelvic pain, hemorrhoids. Ultrasound showed pelvic varices.
- Embolization of pelvic varices was performed with coils only in another hospital, without symptom improvement.
- After consultation at our hospital, a CT scan was requested. That study showed compression of the left renal vein by the mesenteric ligament, compatible with Nutcracker Syndrome.
- Patient underwent left renal venogram and manometry, which showed obstruction of the left renal vein with a gradient of 16 mmHg. Pelvic varices coiling without covering the entire varicose nidus.
After consultation at our hospital, a CT scan was requested. That study showed compression of the left renal vein by the mesenteric ligament compatible with Nutcracker Syndrome.
Patient underwent left renal venogram and manometry, which showed obstruction of the left renal vein with a gradient of 16 mmHg. Pelvic varices coiling was present without covering the entire varicose nidus.
Strategy
Self-expanding venous stent implantation in the left renal vein; disappearance of the gradient and reversal of flow in the left gonadal vein.

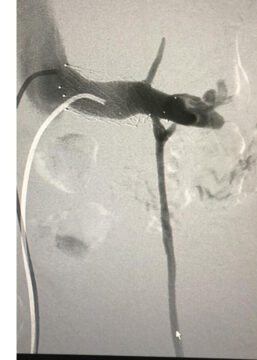
Left renal vein stent
Pelvic varices with coiling from previous treatment before renal vein stenting
Outcome
- The patient remained asymptomatic for 3 months with recurrence of symptoms of dyspareunia and urinary incontinence, in addition to pelvic pain.
- We reevaluated the stent, which remained patent and without gradient.
- We decided to conduct a new embolization with controlled-release microcoils associated with glue (Glubran diluted 1:1, 1:2 and 1:4, finalizing with Onix).
- The patient remains asymptomatic in the 3-year segment.
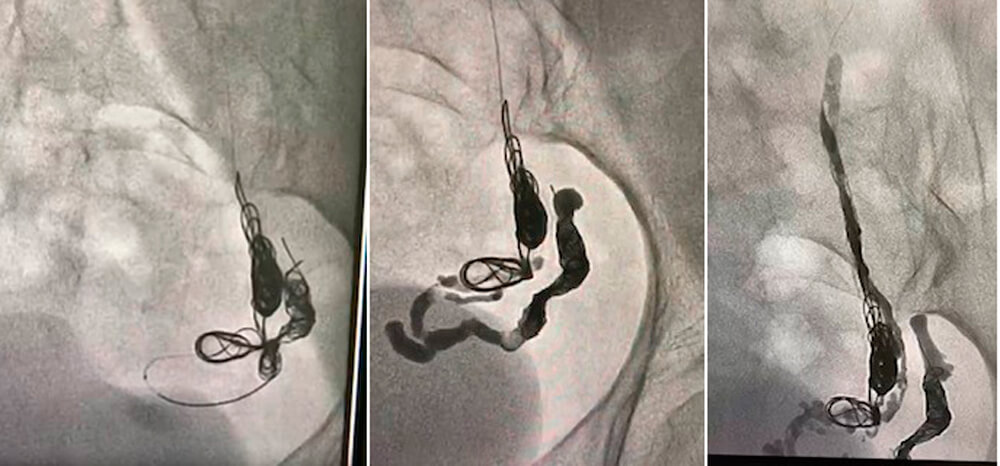
Control angiography after stenting (before new variceal embolization)
Microcatheter placement distal to coils from prior treatment
Angiography after coil release and Glubran (glue)
End result
Questions to guide the discussion
Which is the gold standard diagnostic method for pelvic varices?
- Venogram.
- Computed tomography.
- Magnetic resonance imaging.
- Transvaginal duplex ultrasound.
Which vein is normally used as access to reach the pelvic varicose nidus, which is the vein that should be embolized?
- Left gonadal vein.
- Vena cava.
- Left renal vein.
- Right femoral vein.
Which technique(s) is(are) most effective in preventing recurrence of pelvic varicose veins?
- Renal vein stenting.
- Embolizing most of the varicose nidus and releasing coils along the course of the gonadal vein up to its proximal segment.
- Varicose nidus embolization in its most distal segment with coils.
- Left gonadal vein stenting.
Which is the main symptom caused by pelvic congestion syndrome?
- Infertility.
- Chronic pelvic pain without other clinical causes.
- Increased menstrual bleeding.
- All of the above.
Vea los otros casos clínicos de SOLACI Peripheral publicados en nuestra web.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





