Score to predict the risk of repeat PCI in DES restenosis.
With the use of drug eluting stents (DES) instent restenosis (ISR) has seen a significant reduction vs. bare metal stents (BMS) restenosis.
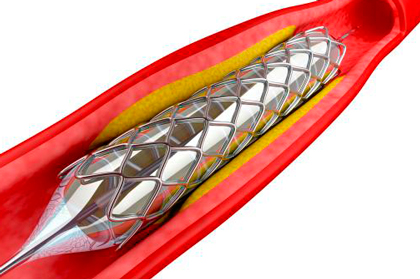
The main cause of DES failure is ISR. This entity is difficult to manage because of its high recurrence and reintervention risk. Even though ISR morphology has been classified (also for prognosis purposes) this classification was based on BMS ISR, which makes us question its value for DES.
In this regard, J.J. Coughlan et all carried out and validated a model to predict the need for repeat PCI in DES ISR, with one-year followup.
Consecutive patients were enrolled since December 2005 to December 2013 at 2 centers in Germany. Based on the Mehran classification, ISR was classified in 4 groups: four groups: type I: focal; type II: diffuse, within stent; type III: diffuse, within and beyond stent; and type IV: occlusive.
Primary end point was repeat PCI for recurrent DES-ISR. Other end points included all-cause mortality, acute MI, stent thrombosis and post ISR CABG.
Read also: Have Complications Related to Balloon Pulmonary Angioplasty Changed Since its Inception?
Retrospectively, patients were randomized 3:1 into training and validation cohorts. Data from 1986 patients treated with PCI for DES-ISR were obtained; 1471 were randomized to the training cohort and 515 to the validation cohort. Mean followup was 7.4 years. Mean age of patients was 69.8 years, 20% were women, 39% diabetic, 25.5% presented as ACS and mean time between first and repeat PCI was 247 days. 65% of cases presented focal ISR, and the most frequent localization was the anterior descending (36.4%), followed by the right coronary (30.3%) and the circumflex (29.3%).
There was accumulated incidence of repeat revascularization with PCI for DES ISR of 17.7% a year. After logistic regression, there were four independent factors leading to repeat PCI: non-focal ISR pattern, a time interval to ISR of <6 months, ISR of the left circumflex and the presence of moderate/severe calcification in target vessel.
These variables were used in the ISAR-SCORE (C-statistic modest con HR 0.60, CI 95%: 0.57-0.63), a point was given to each of the above mentioned factors, with a score ranging between 0 and 4. The annual incidence of repeat PCI for DES ISR 0 score was 12.1%, DES ISR 1 was 15.9%, DES ISR 2 was 24.2% and DES ISR ≥3 was 30.5%. Compared against ISR 0, primary end point incidence increased as follows: Score 1 (HR 1.37, CI 95%: 1.04-1.79), 2 (HR 2.27, CI: 95% 1.69-3.07) y ≥3 (HR 3.11, CI 95%: 2.15-4.81).
Read also: AQCA Study: Pre-PCI Virtual QFR for Planning PCI vs. Conventional Angiography.
ISR score correlated both for ACS (p for trend <0.001) and chronic coronary syndrome (p for trend <0.001).
Conclusions
This study looked at one of the largest cohorts of DES ISR to predict repeat PCI. Based on the presence of 4 factors, researchers were able to develop the ISAR Score. Even though it has a modest discriminatory power, it would allow to identify patients prone to an aggressive response of the treated vessel in the form of restenosis. Further external validation is still required to assess feasibility in the daily practice.

Dr. Omar Tupayachi.
Member of the Editorial Board of SOLACI.org.
Reference: Coughlan, J J et al. “Derivation and validation of the ISAR score to predict the risk of repeat percutaneous coronary intervention for recurrent drug-eluting stent restenosis.” EuroIntervention : journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology vol. 18,16 e1328-e1338. 3 Apr. 2023, doi:10.4244/EIJ-D-22-00860.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology