Original title: Zotarolimus-Eluting Versus Bare-Metal Stents in Uncertain Drug-Eluting Stent Candidates. Reference: Marco Valgimigli et al. J Am Coll Cardiol. 2015;65(8):805-815.
The use of drug eluting stents (DES) in patients at high risk of bleeding or thrombosis has not been studied prospectively. Data on patients at high risk of bleeding and low restenosis are limited.
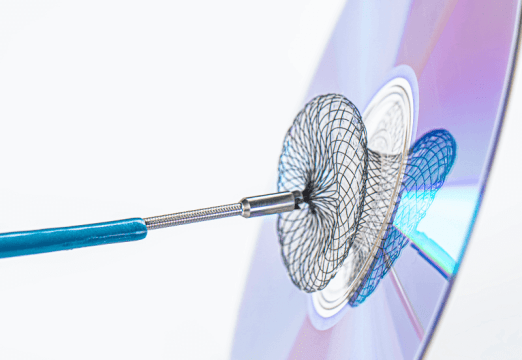
This study compared the second generation zotarolimus eluting stent (ZES) vs. conventional bare metal stents (BMS) in patients receiving dual antiplatelet therapy during a similar period of time (DAPT).
1606 patients with stable or unstable symptoms classified as uncertain candidates for DES based on bleeding and restenosis risk were randomized to BMS. DAPT was decided according to the characteristics of patients, rather than stents.
Primary end point was major adverse events rate at one year, including death, infarction and revascularization. Mean DAPT was 32 days (30 to 180 day range) and was no different between the groups.
In the ZES group, the observed primary end point rate was 17.5% (140 patients) compared to the 22.1% (178 patients) of the BMS group (HR 0.76; CI 95% 0.61 to 0.95; p=0.011) as a result of a lower rate of acute myocardial infarction (2.9% vs 8.1%; p < 0.001) and revascularization of target lesion (5.9% vs.10.7%; p=0.001). Definite /probable thrombosis was also significantly lower with ZES (2.0% vs. 4.1%; p = 0.019).
Conclusion
Compared to conventional stents, a zotarolimus eluting stent with a biocompatible polymer of fast release reduced combined cardiovascular events in uncertain candidates for DES receiving one month DAPT.
Editorial Comment
The difference in revascularization is logical and predictable, when comparing DES vs BMS; however, the significant difference in acute myocardial infarction is more difficult to explain physiopathologically. The mix of stable and unstable patients slightly complicates interpretation, since their differences in thrombosis and bleeding risk are due to their clinical status, not the device.
All patients had high bleeding risk but, at the same time, restenosis risk was relatively low (in fact, they were uncertain candidates for DES). This calls for further research on DAPT in large populations with long lesions, multiple lesions, bifurcations, etc.
SOLACI