3 Year Clinical Outcome Analysis and Failure Predictors in the Use of Intracoronary Brachytherapy for Drug-Eluting Stent Restenosis
In-stent restenosis (ISR) has been one of the greatest obstacles standing in the way of long term patency in percutaneous coronary interventions. However, the use of drug eluting stents (DES) and their development has helped reduce ISR rate significantly. According to US statistics, second generation DES restenosis 5-year rate has been 6%.
Prior to the use of DES (the current treatment of choice for ISR), intracoronary brachytherapy (ICBT) use to be a valid treatment alternative, mainly for bare metal stent ISR. However, the use of this strategy in the DES era has been scarcely looked at.
The US guidelines recommend the use of ICBT with multiple stent layer ISR or when there is unfavorable anatomy for repeat DES (IIB evidence), seeing as the use of drug coated balloons has not yet been approved in this country. The mechanism behind ICBT would be to delay or disrupt the formation of neointima and induce vessel remodeling.
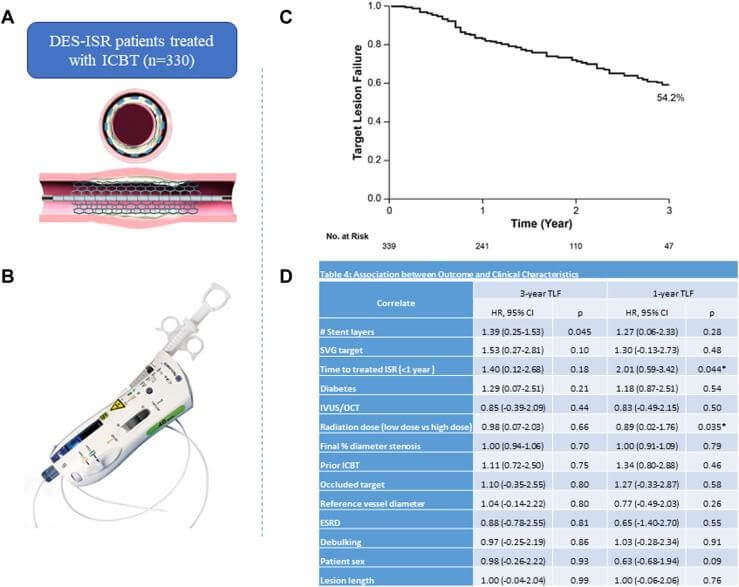
The aim of this study, retrospective and single-centered, carried out by E. Ho, et al., was to report clinical outcomes and correlate ISR predictors in patients with DES ISR treated with ICBT. It included patients between 2010 and 2021, with recurrent angina or confirmed ischemia, either chronic or acute, with DES layer restenosis.
Pretreatment Strategy was determined by the operator (plain old balloon angioplasty, cutting/scoring balloon angioplasty, and laser or rotational atherectomy) and then brachytherapy was performed using Novoste Beta-Cath system (Best Vascular). Doses were considered low with 18.4 Gy (vessels ≤3.35mm) and high with 23 Gy (≥3.35mm).
Read also: Monotherapy with P2Y12 in Complex Interventions: Less and Less Risky.
Primary end point was target lesion failure (TLF) at 3 years, a composite of cardiac mortality, target vessel revascularization, target vessel occlusion or MI. Secondary end points included one year TLF, all-cause mortality and cardiac mortality.
Data from 330 consecutive patients were obtained, mean age 66±11 years, 70.3% mean, 62% with a history of myocardial revascularization surgery (CABG), and 54.4% diabetic. The main clinical scenario was stable angina (only 20.9% MI). Time between stenting and ISR diagnosis was mean 284 days and 88.5% had at least 2 stent layers. The most frequently treated vessel was the anterior descending (29.4%) and most of the treated lesions received 23 Gy (70.8%).
There was 17.7% TLF rate at one year and 45.8% at 3 years, mainly due to increased TLR of 17.5% at one year and 41.7% at 3 years. After regression analysis, there was significant correlation between the number of stent layers and TLF at 3 years (HR 1.39, P=0.045) (60.2% with 3 stent layers). Both low radiation and early ISR correlated with TLF at one year.
Conclusions
In this complex ISR scenario, ICBT was feasible and safe in patients treated with DES. TLF was mainly due to the number of stent layers. Therefore, after placing two DES (avoid placing a third layer), the use of ICBT might be a valid option that should be assessed by future randomized studies.

Dr. Omar Tupayachi.
Member of the Editorial Board of SOLACI.org.
Original Title: Intracoronary Brachytherapy for Drug-Eluting Stent Restenosis: Outcomes and Clinical Correlates.
Reference: Ho E, et Al. Intracoronary Brachytherapy for Drug-Eluting Stent Restenosis: Outcomes and Clinical Correlates. Journal of the Society for Cardiovascular Angiography & Interventions, Volume 2, Issue 1, 2023, https://doi.org/10.1016/j.jscai.2022.100550.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology





