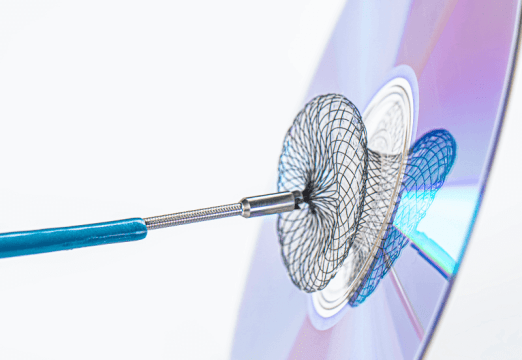
iFR has been validated as a useful tool for intermediate lesion analysis, with the advantage of not requiring the use of drugs. On the other hand, its use for PCI outcome assessment has not yet been thoroughly looked into, even though there have been promising data.
24% of DEFINE PCI cases presented ≤0.89 iFR with a successful angiography. Those reaching ≥0.95 iFR at one year followup, showed lower incidence of cardiovascular mortality, MI, and ischemia driven revascularization.
One analysis of the DEFINE PCI included the assessment of 506 vessels, 61.5% of the left anterior descending (LAD) and 38.5% to non-LAD vessels (99 left coronary, and 96 circumflex). It excluded cases with two vessels, which included the left main.
Primary end point at 12 months was target vessel failure, defined as a composite of cardiovascular death, MI and ischemia driven target vessel revascularization.
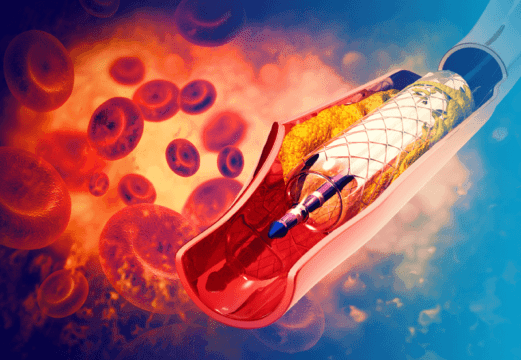
There were no significant differences in bifurcation presence (4%), length (21.2 mm), stent diameter (3.0 mm) or maximum balloon pressure (18 ATM).
Read also: Can Ultrasound Treat Aortic Stenosis?
Calcified lesions in the LAD were more frequent (43.4% vs. 29.7%, p=0.002), reference vessel diameter was shorter (2.73 mm vs 2.84 mm, p<0.0001) and more post-dilation was required (63.8% vs. 51.5%, p=0.007).
Prior to PCI, LAD iFR was higher (0.82 [0.63, 0.86] vs. 0.72 [0.49, 0.84]; p<0.0001). After PCI, there were no angiographic differences in residual lesion, which was 19%.
Suboptimal iFR (<0.95) was higher in the LAD (77.8% vs 22.6%, p<0.0001). The presence of instent focal residual lesions was higher in the LAD (53.7% vs 27.3%, p=0.0009). There were no differences in primary end point at 12 months between the groups.
In both groups, improved iFR after PCI was significantly associated with reduced angina and improved quality of life.
Independent predictors of low iFR after LAD PCI were age, larger body surface and smaller vessels; while in non-LAD lesions, predictors were calcifications and reference vessel diameter.
Conclusion
In conclusion, after PCI with successful PCI, iFR was lower in LAD lesions vs. non-LAD, which resulted in high prevalence of suboptimal iFR in the LAD. This disparity is attributed in part to a higher frequency of focal residual gradient within the stent segment, that might benefit from a more aggressive PCI.

Dr. Carlos Fava.
Member of the Editorial Board of SOLACI.org.
Original Title: Changes in post-PCI physiology based on anatomical vessel location: a DEFINE PCI substudy.
Reference: Mitsuaki Matsumura, et al. EuroIntervention 2023;19-online publish-ahead-of-print November 2023.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology