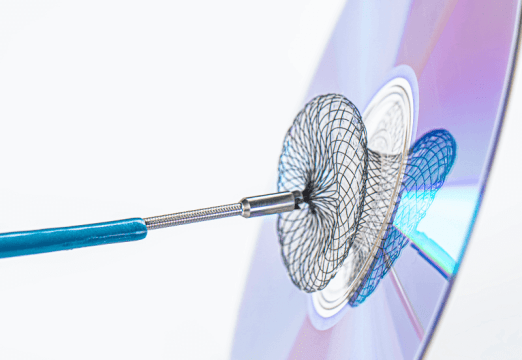
At present, transcatheter aortic valve replacement (TAVR) has become increasingly common to treat severe symptomatic aortic stenosis, with the transfemoral approach being the most common access strategy, associated to better outcomes vs. other access sites. Even though vascular complication rates (VC) have dropped given increased operation experience and improved devices, such as the use of low profile inductors and percutaneous closure devices, they are still associated to higher morbimortality.

The aim of this observational, multicenter, prospective study, was to assess the clinical impact and management of access site vascular complications in patients undergoing TAVR with latest generation devices.
Primary end point was major adverse cardiac and cerebrovascular events (MACCE), defined as a combination of all-cause mortality, stroke, acute myocardial infarction (AMI) and/or coronary revascularization at 1 year. Secondary end point consisted of individual primary end point components, 30-day all-cause mortality, VARC-2 inhospital major bleeding, contrast induced acute kidney failure, inhospital infections and hospital stay.
The study looked at 2504 patients, 337 (13.4%) presenting access site vascular complications. According to VARC-2 criteria, 3.5% were major vascular complications, while 8.7% were minor. Also, 1.3% of patients saw percutaneous closure device failure. Study population was divided in three groups: patients with no VC (No VC group): 2167 patients (86.5%); patients with minor VC and/or percutaneous closure device failure (Minor VC) with 249 patients (9.9%), and patients with major VC (Major VC) with 88 patients (3.5%). There were fewer women among No VC patients, vs. Minor VC and Major VC (55% vs. 63% vs. 65%, p = 0.02) and there were no significant differences in EuroScore II between the three groups.
Read also: Calcified Nodules and the Importance of OCT Categorization prior PCI.
With regard to the primary end point, Minor VC patients presented comparable risk vs. No VC patients, while Major VC patients saw significantly worse outcomes (p = 0.003) mainly driven by major mortality vs. Minor VC and No VC (22% vs. 7% vs. 11%, p < 0.0001). 30-day all-cause mortality was also higher among Major VC patients vs. the other two groups (p < 0.0001). Moreover, there was higher incidence of contrast induced acute kidney failure, major inhospital bleeding and longer hospital stay among Major VC patients.
Conclusion
Though these outcomes show lower incidence of major vascular complications [vs. earlier devices], these are still associated with worse clinical outcomes. Therefore, we need to optimize patient selection and imaging-based planning to further reduce VC incidence after TAVR.
Dr. Andrés Rodríguez.
Member of the Editorial Board of SOLACI.org.
Original Title: Impact of vascular complications after transcatheter aortic valve implantation. VASC‐OBSERVANT II sub‐study.
Reference: Cristina Aurigemma MD, PhD et al Catheter Cardiovasc Interv. 2023;1–11.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology