Cardiogenic shock (CS) in a setting of aortic stenosis is associated with high mortality rates. In consequence, surgery is generally not a possibility for this patient group, and they usually undergo aortic valvuloplasty, resulting in a mortality rate of 33%-50% at 30 days, 70% at one year, and 90% at two years.
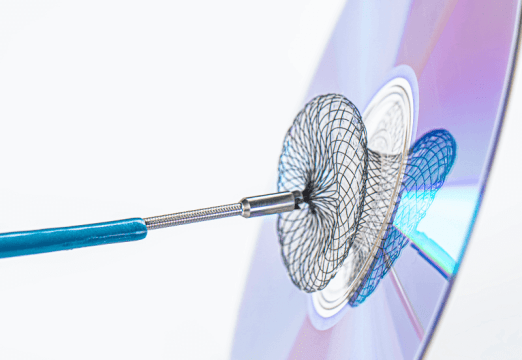
While transcatheter aortic valve replacement (TAVR) has shown benefits, only a small group of patients receive this treatment in this scenario (1%-4%), and evidence is limited, especially with first-generation valves, the most used type. Increasing operator experience and further technological development of current valves will most likely ensure better results than those offered by previous series.
Researchers conducted an analysis of the STS/ACC-TVT Registry, which included 309,505 consecutive patients who received balloon-expandable SAPIEN 3 or SAPIEN ULTRA valve between June 2015 and September 2020. Of these patients, 5006 (1.6%) were in cardiogenic shock.
The Primary Endpoint (PEP) was all-cause mortality at one year.
Patients with cardiogenic shock were younger (75.5 vs. 78.9, p=<0.0001), and most of them were men. They had a higher incidence of hypertension, diabetes, chronic obstructive pulmonary disease (COPD), oxygen dependence at home, stroke, impaired renal function, dialysis, atrial fibrillation, coronary artery disease, heart attack, percutaneous coronary intervention (PCI), myocardial revascularization surgery (MRS), aortic valve replacement, V-in-V, and peripheral vascular disease.
Ejection fraction in these patients was lower, and so were the aortic valve area and the mean gradient. Additionally, there was a higher presence of moderate to severe mitral and tricuspid regurgitation.
Surgical risk, analyzed based on the STS score, was higher in patients with cardiogenic shock (10.7% vs. 4.88%, p<0.001).
Technical success was higher in patients without cardiogenic shock (96.7% vs. 94.5%, p<0.0001).
At 30 days, patients with cardiogenic shock had higher mortality (9.9% vs. 2.7%; odds ratio [OR] 3.64, 95% confidence interval [CI] 3.02-4.39; p<0.0001) and higher incidence of cardiovascular mortality, stroke, need for dialysis, major vascular complications, major bleeding, atrial fibrillation, PCI, and coronary occlusion.
Read also: Post PCI Functional Assessment for Focal Lesion and Stent Underexpansion Detection.
The PEP at one year was higher in patients who had cardiogenic shock (29.7% vs. 22.6%; hazard ratio (HR) 1.57; 95% CI: 1.43-1.72; p < 0.001). Additionally, there was a higher incidence of stroke, atrial fibrillation, major bleeding, need for dialysis, major vascular complications, and PCI in this group. There were no significant differences in the need for permanent pacemaker (9.3% vs. 9.1%), reintervention, or TAVR-related hospitalization.
After one year, all patients had experienced improvement in their functional class and quality of life, with no significant differences between groups.
The predictors of mortality were age, peripheral vascular disease, cardioverter-defibrillator implantation, need for dialysis, immunosuppression, functional class III-IV, low mean gradient, albumin levels, hemoglobin, and quality of life (KCCQ).
Conclusion
In conclusion, this extensive observational “real-world” registry demonstrated the safety and efficacy of TAVR in the treatment of aortic stenosis with cardiogenic shock. Patients who survived the first 30 days after the TAVR procedure had a mortality rate similar to that of patients who did not experience cardiogenic shock.

Dr. Carlos Fava.
Member of the Editorial Board of SOLACI.org.
Original Title: Outcomes of transcatheter aortic valve replacement in patients with cardiogenic shock.
Reference: Kashish Goel, et al. European Heart Journal (2023) 00, 1–15 https://doi.org/10.1093/eurheartj/ehad387.
Subscribe to our weekly newsletter
Get the latest scientific articles on interventional cardiology